Sunday Poster Session
Category: GI Bleeding
P0656 - Successful Treatment of Refractory Small Intestinal Angioectasias with Bevacizumab: A Novel Therapeutic Approach
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aishwarya Thakurdesai, MBBS, MD
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Award: Presidential Poster Award
Aishwarya Thakurdesai, MBBS, MD, Lucia Rivera-Matos, MD, Amal Shine, MD, Dipendra Parajuli, MD
University of Louisville School of Medicine, Louisville, KY
Introduction: Angioectasias (AEs) are vascular lesions commonly seen in the elderly and account for 5-10% of all gastrointestinal (GI) bleeds. Unlike arteriovenous malformations (AVMs), AEs are neither congenital nor associated with skin/visceral lesions. AEs express vascular endothelial growth factor (VEGF) and its receptors. Bevacizumab is a VEGF inhibitor used to treat AVMs in patients with hereditary hemorrhagic telangiectasia (HHT). We describe a case of non-hereditary GI AEs refractory to multiple therapies, successfully treated with Bevacizumab.
Case Description/Methods: An 82-year-old male with a history of atrial fibrillation and chronic kidney disease was being followed in GI clinic for persistent iron deficiency anemia [hemoglobin (Hb) 6-8 gm/dL] due to recurrent bleeding GI AEs. He underwent multiple endoscopic procedures over 2 years including esophagogastroduodenoscopies, capsule endoscopies, and push enteroscopies showing recurrent bleeding small bowel AEs despite repeated treatment with argon plasma coagulation (APC). He continued to have intermittent melena, requiring either iron infusions for ferritin less than (< ) 50 ng/mL or blood transfusions for Hb < 7 gm/dL every 2 weeks. He then opted for medical therapy. Thalidomide and Octreotide were trialed with poor response. He was then transitioned to 2-weekly Bevacizumab infusions of 5mg/kg. Hb gradually improved to more than ( >) 12 gm/dL with ferritin maintained above 50 ng/mL. After 8 bimonthly doses, he was changed to a monthly schedule. However, Hb dropped again to 8 gm/dL and bimonthly Bevacizumab infusions were thus restarted, followed by improvement. Apixaban for atrial fibrillation was able to be resumed. As of most recent follow up, his Hb remains > 12 gm/dL without further melena or transfusion requirements.
Discussion: Bevacizumab is a recombinant monoclonal antibody that inhibits VEGF. Multiple studies in HHT have reported treatment success with Bevacizumab. The InHIBIT-Bleed Study, a multicenter, retrospective study, showed increased mean hemoglobin by 3.2 gm/dL in the 1st year and decreased number of units transfused by 82% during the first 6 months after treatment with Bevacizumab. In our patient, it was hypothesized that Bevacizumab would be effective in treating non-hereditary refractory GI AEs. Dosage regimens were extrapolated from the InHIBIT-Bleed Study with an excellent response. Bevacizumab may thus be effective in treatment of GI AEs but randomized controlled trials are needed in this area to assess its true effect.

Disclosures:
Aishwarya Thakurdesai, MBBS, MD, Lucia Rivera-Matos, MD, Amal Shine, MD, Dipendra Parajuli, MD. P0656 - Successful Treatment of Refractory Small Intestinal Angioectasias with Bevacizumab: A Novel Therapeutic Approach, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Aishwarya Thakurdesai, MBBS, MD, Lucia Rivera-Matos, MD, Amal Shine, MD, Dipendra Parajuli, MD
University of Louisville School of Medicine, Louisville, KY
Introduction: Angioectasias (AEs) are vascular lesions commonly seen in the elderly and account for 5-10% of all gastrointestinal (GI) bleeds. Unlike arteriovenous malformations (AVMs), AEs are neither congenital nor associated with skin/visceral lesions. AEs express vascular endothelial growth factor (VEGF) and its receptors. Bevacizumab is a VEGF inhibitor used to treat AVMs in patients with hereditary hemorrhagic telangiectasia (HHT). We describe a case of non-hereditary GI AEs refractory to multiple therapies, successfully treated with Bevacizumab.
Case Description/Methods: An 82-year-old male with a history of atrial fibrillation and chronic kidney disease was being followed in GI clinic for persistent iron deficiency anemia [hemoglobin (Hb) 6-8 gm/dL] due to recurrent bleeding GI AEs. He underwent multiple endoscopic procedures over 2 years including esophagogastroduodenoscopies, capsule endoscopies, and push enteroscopies showing recurrent bleeding small bowel AEs despite repeated treatment with argon plasma coagulation (APC). He continued to have intermittent melena, requiring either iron infusions for ferritin less than (< ) 50 ng/mL or blood transfusions for Hb < 7 gm/dL every 2 weeks. He then opted for medical therapy. Thalidomide and Octreotide were trialed with poor response. He was then transitioned to 2-weekly Bevacizumab infusions of 5mg/kg. Hb gradually improved to more than ( >) 12 gm/dL with ferritin maintained above 50 ng/mL. After 8 bimonthly doses, he was changed to a monthly schedule. However, Hb dropped again to 8 gm/dL and bimonthly Bevacizumab infusions were thus restarted, followed by improvement. Apixaban for atrial fibrillation was able to be resumed. As of most recent follow up, his Hb remains > 12 gm/dL without further melena or transfusion requirements.
Discussion: Bevacizumab is a recombinant monoclonal antibody that inhibits VEGF. Multiple studies in HHT have reported treatment success with Bevacizumab. The InHIBIT-Bleed Study, a multicenter, retrospective study, showed increased mean hemoglobin by 3.2 gm/dL in the 1st year and decreased number of units transfused by 82% during the first 6 months after treatment with Bevacizumab. In our patient, it was hypothesized that Bevacizumab would be effective in treating non-hereditary refractory GI AEs. Dosage regimens were extrapolated from the InHIBIT-Bleed Study with an excellent response. Bevacizumab may thus be effective in treatment of GI AEs but randomized controlled trials are needed in this area to assess its true effect.

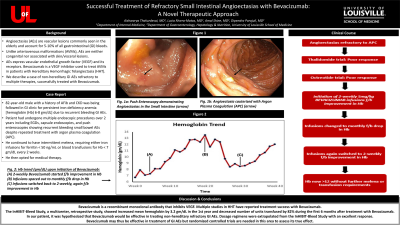
Figure: Hemoglobin trend (gm/dL) upon initiation of Bevacizumab Therapy:
(A) 2-weekly Bevacizumab infusions started followed by improvement in Hemoglobin
(B, C) Infusions spaced out to monthly followed by drop in Hemoglobin
(D) Infusions switched back to 2-weekly, again followed by improvement in Hemoglobin
(A) 2-weekly Bevacizumab infusions started followed by improvement in Hemoglobin
(B, C) Infusions spaced out to monthly followed by drop in Hemoglobin
(D) Infusions switched back to 2-weekly, again followed by improvement in Hemoglobin
Disclosures:
Aishwarya Thakurdesai indicated no relevant financial relationships.
Lucia Rivera-Matos indicated no relevant financial relationships.
Amal Shine indicated no relevant financial relationships.
Dipendra Parajuli indicated no relevant financial relationships.
Aishwarya Thakurdesai, MBBS, MD, Lucia Rivera-Matos, MD, Amal Shine, MD, Dipendra Parajuli, MD. P0656 - Successful Treatment of Refractory Small Intestinal Angioectasias with Bevacizumab: A Novel Therapeutic Approach, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

