Sunday Poster Session
Category: GI Bleeding
P0658 - An Unusual Presentation of Von Hippel-Lindau Syndrome With Gastric Variceal Bleeding
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

David Graham, MD
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
David Graham, MD1, Blake Thompson, MD1, Parvez Mantry, MD2
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Liver Institute, Dallas, TX
Introduction: This is an interesting case of gastrointestinal bleeding from gastric varices related to cirrhosis and splenic vein thrombosis from chronic pancreatitis with pancreatic neuroendocrine tumor in a patient diagnosed with von Hippel-Lindau (VHL) disease.
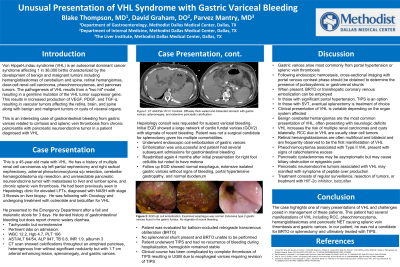
Case Description/Methods: We present a 45 year-old male with VHL. He has a history of multiple renal cell carcinomas s/p left partial nephrectomy and right radical nephrectomy, adrenal pheochromocytoma s/p resection, cerebellar hemangioblastoma s/p resection, and unresectable pancreatic neuroendocrine tumor with metastasis to liver and lumbar spine.
He presented after a fall while using the restroom and melanotic stools over 3 days. Labs with WBC 12.2, Hgb 4.7, PLT 106, AST/ALT 64/54, ALP 947, TB 0.8, INR 1.9, albumin 3.1. Computerized tomography (CT) scan showed calcifications throughout an atrophied pancreas, splenic vein thrombosis (SVT), portal vein thrombosis (PVT), a cirrhotic appearing liver with enhancing lesions throughout, splenomegaly and varices.
A hepatology consult was requested for suspect variceal bleeding. EGD showed a large network of cardiofundal varices (GOV2) with stigmata of recent bleeding. Patient was not a surgical candidate for splenectomy given his multiple comorbidities, and no gastrorenal shunt was present for balloon-occluded retrograde transvenous obliteration (BRTO). Thus, upper endoscopic ultrasound was performed with coiling of the gastric varices. Patient was later readmitted for bleeding and a TIPS was placed.
Discussion: VHL is an autosomal dominant syndrome affecting 1 in 36,000 births characterized by hemangioblastomas of cerebellum and spine, retinal hemangiomas, clear-cell renal cell carcinoma, pheochromocytomas, and pancreas tumors.
Gastric varices arise most commonly from portal hypertension or splenic vein thrombosis. Following endoscopic hemostasis, cross-sectional imaging with portal venous contrast phase should be obtained to determine the presence of portosystemic or gastrorenal shunts. When present, BRTO or transhepatic coronary venous embolization can be employed. In those with significant portal hypertension, TIPS is an option. In those with SVT, eventual splenectomy is treatment of choice.
In our patient, he was not a candidate for TIPS, BRTO or splenectomy. We pursued definitive therapy with EUS-guided coil embolization with subsequent cessation of Doppler flow in the gastric variceal nest.
The case highlights one of many presentations of VHL and challenges posed in management of these patients.
Disclosures:
David Graham, MD1, Blake Thompson, MD1, Parvez Mantry, MD2. P0658 - An Unusual Presentation of Von Hippel-Lindau Syndrome With Gastric Variceal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Liver Institute, Dallas, TX
Introduction: This is an interesting case of gastrointestinal bleeding from gastric varices related to cirrhosis and splenic vein thrombosis from chronic pancreatitis with pancreatic neuroendocrine tumor in a patient diagnosed with von Hippel-Lindau (VHL) disease.
Case Description/Methods: We present a 45 year-old male with VHL. He has a history of multiple renal cell carcinomas s/p left partial nephrectomy and right radical nephrectomy, adrenal pheochromocytoma s/p resection, cerebellar hemangioblastoma s/p resection, and unresectable pancreatic neuroendocrine tumor with metastasis to liver and lumbar spine.
He presented after a fall while using the restroom and melanotic stools over 3 days. Labs with WBC 12.2, Hgb 4.7, PLT 106, AST/ALT 64/54, ALP 947, TB 0.8, INR 1.9, albumin 3.1. Computerized tomography (CT) scan showed calcifications throughout an atrophied pancreas, splenic vein thrombosis (SVT), portal vein thrombosis (PVT), a cirrhotic appearing liver with enhancing lesions throughout, splenomegaly and varices.
A hepatology consult was requested for suspect variceal bleeding. EGD showed a large network of cardiofundal varices (GOV2) with stigmata of recent bleeding. Patient was not a surgical candidate for splenectomy given his multiple comorbidities, and no gastrorenal shunt was present for balloon-occluded retrograde transvenous obliteration (BRTO). Thus, upper endoscopic ultrasound was performed with coiling of the gastric varices. Patient was later readmitted for bleeding and a TIPS was placed.
Discussion: VHL is an autosomal dominant syndrome affecting 1 in 36,000 births characterized by hemangioblastomas of cerebellum and spine, retinal hemangiomas, clear-cell renal cell carcinoma, pheochromocytomas, and pancreas tumors.
Gastric varices arise most commonly from portal hypertension or splenic vein thrombosis. Following endoscopic hemostasis, cross-sectional imaging with portal venous contrast phase should be obtained to determine the presence of portosystemic or gastrorenal shunts. When present, BRTO or transhepatic coronary venous embolization can be employed. In those with significant portal hypertension, TIPS is an option. In those with SVT, eventual splenectomy is treatment of choice.
In our patient, he was not a candidate for TIPS, BRTO or splenectomy. We pursued definitive therapy with EUS-guided coil embolization with subsequent cessation of Doppler flow in the gastric variceal nest.
The case highlights one of many presentations of VHL and challenges posed in management of these patients.
Disclosures:
David Graham indicated no relevant financial relationships.
Blake Thompson indicated no relevant financial relationships.
Parvez Mantry indicated no relevant financial relationships.
David Graham, MD1, Blake Thompson, MD1, Parvez Mantry, MD2. P0658 - An Unusual Presentation of Von Hippel-Lindau Syndrome With Gastric Variceal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
