Sunday Poster Session
Category: GI Bleeding
P0660 - A Rare Case of High-Volume Appendiceal Bleed From a Colostomy: Management Challenges of an Unforeseen Hemorrhage
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- SK
Saurav Kini, MBBS
Tufts Medical Center
Boston, MA
Presenting Author(s)
Saurav A. Kini, MBBS1, Anjali Rajagopal, MBBS2
1Tufts Medical Center, Boston, MA; 2Mayo Clinic, Rochester, MN
Introduction: Lower gastrointestinal (GI) bleeding from the appendix is an extremely rare clinical entity that can prove potentially life-threatening. There is a paucity of literature on high-volume appendiceal bleeds and no established management guidelines at present. Herein we present a case of appendiceal bleeding highlighting complexities in diagnosis and management.
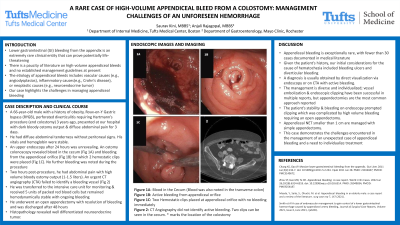
Case Description/Methods: A 66-year-old male with a history of obesity, Roux-en-Y Gastric bypass (RYGB), perforated diverticulitis requiring Hartmann’s procedure (end colostomy) 3 years ago, presented at our hospital with dark bloody ostomy output & diffuse abdominal pain for 3 days. He had diffuse abdominal tenderness without peritoneal signs. His vitals and hemoglobin were stable. An endoscopy performed after 24 hours was unrevealing. An ostomy colonoscopy revealed blood in the cecum (Fig 1A) and bleeding from the appendiceal orifice (Fig 1B) for which 2 hemostatic clips were placed (Fig 1C) No further bleeding was noted during the procedure. Two hours post-procedure, he had abdominal pain with high volume bloody ostomy output (1-1.5 liters). This prompted an urgent CT angiography (CTA) that failed to identify a bleeding vessel for possible embolization. (Fig 2) He was transferred to the intensive care unit for monitoring & received 5 units of packed red blood cells but remained hemodynamically stable. He underwent an open appendectomy with resolution of bleeding and was discharged after 48 hours.
Discussion: Appendiceal bleeding is exceptionally rare, with fewer than 30 cases documented in medical literature. The etiology of appendiceal bleeds can be vascular (angiodysplasias), inflammatory (Crohn’s disease), or neoplastic. Given the patient's history, our initial considerations for the cause of hematochezia included bleeding ulcers and diverticular bleeding. A diagnosis is usually obtained by direct visualization via endoscopy or on CTA with active bleeding. The management is diverse and individualized; vessel embolization & endoscopic clipping have been successful, but appendectomies are the most common approach reported. In our case, the patient’s stability & bleeding on endoscopy prompted clipping which was complicated by high volume bleeding requiring an open appendectomy. We suspect a vascular cause but are awaiting final histopathology at the time of submission. This case demonstrates the challenges encountered in the management of an unexpected case of appendiceal bleeding and an urgent need to study treatment options.

Disclosures:
Saurav A. Kini, MBBS1, Anjali Rajagopal, MBBS2. P0660 - A Rare Case of High-Volume Appendiceal Bleed From a Colostomy: Management Challenges of an Unforeseen Hemorrhage, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Mayo Clinic, Rochester, MN
Introduction: Lower gastrointestinal (GI) bleeding from the appendix is an extremely rare clinical entity that can prove potentially life-threatening. There is a paucity of literature on high-volume appendiceal bleeds and no established management guidelines at present. Herein we present a case of appendiceal bleeding highlighting complexities in diagnosis and management.
Case Description/Methods: A 66-year-old male with a history of obesity, Roux-en-Y Gastric bypass (RYGB), perforated diverticulitis requiring Hartmann’s procedure (end colostomy) 3 years ago, presented at our hospital with dark bloody ostomy output & diffuse abdominal pain for 3 days. He had diffuse abdominal tenderness without peritoneal signs. His vitals and hemoglobin were stable. An endoscopy performed after 24 hours was unrevealing. An ostomy colonoscopy revealed blood in the cecum (Fig 1A) and bleeding from the appendiceal orifice (Fig 1B) for which 2 hemostatic clips were placed (Fig 1C) No further bleeding was noted during the procedure. Two hours post-procedure, he had abdominal pain with high volume bloody ostomy output (1-1.5 liters). This prompted an urgent CT angiography (CTA) that failed to identify a bleeding vessel for possible embolization. (Fig 2) He was transferred to the intensive care unit for monitoring & received 5 units of packed red blood cells but remained hemodynamically stable. He underwent an open appendectomy with resolution of bleeding and was discharged after 48 hours.
Discussion: Appendiceal bleeding is exceptionally rare, with fewer than 30 cases documented in medical literature. The etiology of appendiceal bleeds can be vascular (angiodysplasias), inflammatory (Crohn’s disease), or neoplastic. Given the patient's history, our initial considerations for the cause of hematochezia included bleeding ulcers and diverticular bleeding. A diagnosis is usually obtained by direct visualization via endoscopy or on CTA with active bleeding. The management is diverse and individualized; vessel embolization & endoscopic clipping have been successful, but appendectomies are the most common approach reported. In our case, the patient’s stability & bleeding on endoscopy prompted clipping which was complicated by high volume bleeding requiring an open appendectomy. We suspect a vascular cause but are awaiting final histopathology at the time of submission. This case demonstrates the challenges encountered in the management of an unexpected case of appendiceal bleeding and an urgent need to study treatment options.

Figure: Figure 1 A: Blood in the Cecum (Blood was also noted in the transverse colon)
Figure 1 B: Active bleeding from appendiceal orifice
Figure 1 C: Two Hemostatic clips placed at appendiceal orifice with no bleeding immediately
Figure 2: CT Angiography with no active arterial bleeding. Two clips can been seen in the cecum.
Figure 1 B: Active bleeding from appendiceal orifice
Figure 1 C: Two Hemostatic clips placed at appendiceal orifice with no bleeding immediately
Figure 2: CT Angiography with no active arterial bleeding. Two clips can been seen in the cecum.
Disclosures:
Saurav Kini indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
Saurav A. Kini, MBBS1, Anjali Rajagopal, MBBS2. P0660 - A Rare Case of High-Volume Appendiceal Bleed From a Colostomy: Management Challenges of an Unforeseen Hemorrhage, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
