Sunday Poster Session
Category: GI Bleeding
P0663 - Chasing an Elusive Diagnosis of Adult IgA Vasculitis With Gastrointestinal Involvement
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Sandy Vien, MD
University of California, Davis Medical Center
Sacramento, California
Presenting Author(s)
Sandy Vien, MD, Christine Shieh, MD, Karen Matsukuma, MD, PhD, Jeffrey Ko, MD, Kuldeep Tagore, MD
University of California, Davis Medical Center, Sacramento, CA
Introduction: Immunoglobulin A vasculitis (IgAV) is a rare systemic vasculitis that is challenging to diagnose in patients with isolated gastrointestinal manifestations due to variable clinical symptoms and endoscopic findings as well as disease mimickers. We present a case of IgAV in an immunosuppressed male who underwent serologic testing, imaging, and multiple endoscopies during a prolonged hospitalization before arriving at the diagnosis of IgAV.
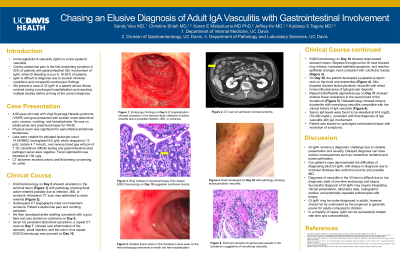
Case Description/Methods: A 66-year-old male with Vogt-Koyanagi-Harada syndrome (VKHS) and gout presented with acute abdominal pain, vomiting, and hematochezia. He was on adalimumab and a prednisone taper for VKHS. Initial workup revealed leukocytosis, mild anemia, and elevated fecal calprotectin with negative stool infectious studies. CT scan showed colonic wall thickening concerning for colitis. Patient underwent an upper endoscopy and colonoscopy which showed terminal ileitis with pathology showing focal active enteritis (Fig 1A).
The patient’s hematochezia resolved but his abdominal pain persisted. He developed acute gout of the ankle and was started on colchicine. Repeat CT on Day 7 showed inflammation in the stomach, small intestine, and colon. Repeat upper endoscopy and colonoscopy with biopsies showed ring mitoses and epithelial apoptosis consistent with colchicine toxicity (Fig 1B).
On Day 30 of his hospitalization, patient developed a palpable purpuric rash with biopsies showing leukocytoclastic vasculitis with IgA granular deposits. A third upper endoscopy and sigmoidoscopy was performed which showed shallow linear ulcerations in the duodenum with pathology showing necrotizing vasculitis (Fig 1C and 1D). Serum IgA levels were elevated at 614 (70-400 mg/dL), consistent with IgAV. Patient was started on corticosteroids with resolution of symptoms.
Discussion: Gut IgAV remains a diagnostic challenge for clinicians given the wide range of symptoms which can lead to delayed diagnosis. This is one of the few cases where IgAV manifested as an idiosyncratic reaction in a patient on adalimumab with no other identifying triggers. Our case illustrates several mimickers of IgAV such as Crohn’s disease, gut ischemia, and colchicine toxicity. It also highlights the importance of readdressing new clinical symptoms with repeat imaging and endoscopy if necessary. In the majority of cases, IgAV can be treated successfully with a corticosteroid taper if diagnosed in a timely manner.

Disclosures:
Sandy Vien, MD, Christine Shieh, MD, Karen Matsukuma, MD, PhD, Jeffrey Ko, MD, Kuldeep Tagore, MD. P0663 - Chasing an Elusive Diagnosis of Adult IgA Vasculitis With Gastrointestinal Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of California, Davis Medical Center, Sacramento, CA
Introduction: Immunoglobulin A vasculitis (IgAV) is a rare systemic vasculitis that is challenging to diagnose in patients with isolated gastrointestinal manifestations due to variable clinical symptoms and endoscopic findings as well as disease mimickers. We present a case of IgAV in an immunosuppressed male who underwent serologic testing, imaging, and multiple endoscopies during a prolonged hospitalization before arriving at the diagnosis of IgAV.
Case Description/Methods: A 66-year-old male with Vogt-Koyanagi-Harada syndrome (VKHS) and gout presented with acute abdominal pain, vomiting, and hematochezia. He was on adalimumab and a prednisone taper for VKHS. Initial workup revealed leukocytosis, mild anemia, and elevated fecal calprotectin with negative stool infectious studies. CT scan showed colonic wall thickening concerning for colitis. Patient underwent an upper endoscopy and colonoscopy which showed terminal ileitis with pathology showing focal active enteritis (Fig 1A).
The patient’s hematochezia resolved but his abdominal pain persisted. He developed acute gout of the ankle and was started on colchicine. Repeat CT on Day 7 showed inflammation in the stomach, small intestine, and colon. Repeat upper endoscopy and colonoscopy with biopsies showed ring mitoses and epithelial apoptosis consistent with colchicine toxicity (Fig 1B).
On Day 30 of his hospitalization, patient developed a palpable purpuric rash with biopsies showing leukocytoclastic vasculitis with IgA granular deposits. A third upper endoscopy and sigmoidoscopy was performed which showed shallow linear ulcerations in the duodenum with pathology showing necrotizing vasculitis (Fig 1C and 1D). Serum IgA levels were elevated at 614 (70-400 mg/dL), consistent with IgAV. Patient was started on corticosteroids with resolution of symptoms.
Discussion: Gut IgAV remains a diagnostic challenge for clinicians given the wide range of symptoms which can lead to delayed diagnosis. This is one of the few cases where IgAV manifested as an idiosyncratic reaction in a patient on adalimumab with no other identifying triggers. Our case illustrates several mimickers of IgAV such as Crohn’s disease, gut ischemia, and colchicine toxicity. It also highlights the importance of readdressing new clinical symptoms with repeat imaging and endoscopy if necessary. In the majority of cases, IgAV can be treated successfully with a corticosteroid taper if diagnosed in a timely manner.

Figure: Figure 1 shows the evolving endoscopic findings of this case. Panel A shows terminal ileitis found on the first colonoscopy. Panel B shows ringed mitoses from repeat upper endoscopy and colonoscopy biopsies most consistent with colchicine toxicity. Panel C shows shallow linear ulcers in the duodenum which was found on the third upper endoscopy performed a month into the hospitalization with histopathology in Panel D showing fibrinoid necrosis of the submucosal vessels, suggestive of necrotizing vasculitis.
Disclosures:
Sandy Vien indicated no relevant financial relationships.
Christine Shieh indicated no relevant financial relationships.
Karen Matsukuma indicated no relevant financial relationships.
Jeffrey Ko indicated no relevant financial relationships.
Kuldeep Tagore indicated no relevant financial relationships.
Sandy Vien, MD, Christine Shieh, MD, Karen Matsukuma, MD, PhD, Jeffrey Ko, MD, Kuldeep Tagore, MD. P0663 - Chasing an Elusive Diagnosis of Adult IgA Vasculitis With Gastrointestinal Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
