Sunday Poster Session
Category: GI Bleeding
P0664 - Metal Biliary Stent Migration: An Unexpected Cause of Hemorrhagic Shock
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Sarah Burroughs, DO
NorthShore University Health System
Evanston, IL
Presenting Author(s)
Sarah Burroughs, DO, Michael Sprang, MD
NorthShore University Health System, Evanston, IL
Introduction: Self expandible metal stents (SEMS) are often placed for biliary drainage. While stent migration can occur, few cases of biliary stent migration into the colon have been reported. To our knowledge, this is the first case of biliary stent migration to the rectum resulting in hemorrhagic shock and perforation.
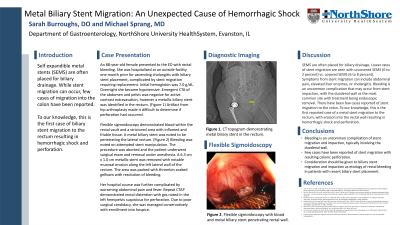
Case Description/Methods: An 88-year-old female with history of pulmonary embolism on apixaban presented to the ED with rectal bleeding. She was hospitalized at an outside facility one month prior for ascending cholangitis with biliary stent placement, complicated by stent migration requiring replacement. Initial hemoglobin was 7.0 g/dL and platelets 67 K/uL. Overnight she became hypotensive. Emergent CTA of the abdomen and pelvis was negative for active contrast extravasation in the GI tract, however a metallic biliary stent was identified in the rectum. Artifact from a prior hip arthroplasty made it difficult to determine if perforation had occurred. Flexible sigmoidoscopy demonstrated blood within the rectal vault and a strictured area with inflamed and friable tissue. A metal biliary stent was noted to be penetrating the lateral rectum with possible fat visualization. (Figure 1) Frank bleeding was noted on attempted stent manipulation. The procedure was aborted and the patient was taken to the OR for surgical exam and removal under anesthesia. A 6.3 cm x 1.0 cm metallic stent was removed with notable mucosal erosion along the left lateral wall of the rectum. The area was packed with thrombin soaked gelfoam with resolution of bleeding. Her hospital course was further complicated by worsening abdominal pain and fever. Repeat CTAP demonstrated rectal distention with gas noted in the left hemipelvis suspicious for perforation. Due to poor surgical candidacy, she was managed conservatively with enrollment into hospice.
Discussion: SEMS are often placed for biliary drainage. Lower rates of stent migration are seen with uncovered SEMS (0 to 2 percent) vs. covered SEMS (6 to 8 percent). Symptoms from stent migration can include abdominal pain, elevated liver enzymes, or cholangitis. Bleeding is an uncommon complication that may occur from stent impaction, with the duodenal wall as the most common site with treatment being endoscopic removal. There have been few cases reported of stent migration to the colon. To our knowledge, this is the first reported case of a metal stent migration to the rectum, with erosion into the rectal wall resulting in hemorrhagic shock and perforation.

Disclosures:
Sarah Burroughs, DO, Michael Sprang, MD. P0664 - Metal Biliary Stent Migration: An Unexpected Cause of Hemorrhagic Shock, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
NorthShore University Health System, Evanston, IL
Introduction: Self expandible metal stents (SEMS) are often placed for biliary drainage. While stent migration can occur, few cases of biliary stent migration into the colon have been reported. To our knowledge, this is the first case of biliary stent migration to the rectum resulting in hemorrhagic shock and perforation.
Case Description/Methods: An 88-year-old female with history of pulmonary embolism on apixaban presented to the ED with rectal bleeding. She was hospitalized at an outside facility one month prior for ascending cholangitis with biliary stent placement, complicated by stent migration requiring replacement. Initial hemoglobin was 7.0 g/dL and platelets 67 K/uL. Overnight she became hypotensive. Emergent CTA of the abdomen and pelvis was negative for active contrast extravasation in the GI tract, however a metallic biliary stent was identified in the rectum. Artifact from a prior hip arthroplasty made it difficult to determine if perforation had occurred. Flexible sigmoidoscopy demonstrated blood within the rectal vault and a strictured area with inflamed and friable tissue. A metal biliary stent was noted to be penetrating the lateral rectum with possible fat visualization. (Figure 1) Frank bleeding was noted on attempted stent manipulation. The procedure was aborted and the patient was taken to the OR for surgical exam and removal under anesthesia. A 6.3 cm x 1.0 cm metallic stent was removed with notable mucosal erosion along the left lateral wall of the rectum. The area was packed with thrombin soaked gelfoam with resolution of bleeding. Her hospital course was further complicated by worsening abdominal pain and fever. Repeat CTAP demonstrated rectal distention with gas noted in the left hemipelvis suspicious for perforation. Due to poor surgical candidacy, she was managed conservatively with enrollment into hospice.
Discussion: SEMS are often placed for biliary drainage. Lower rates of stent migration are seen with uncovered SEMS (0 to 2 percent) vs. covered SEMS (6 to 8 percent). Symptoms from stent migration can include abdominal pain, elevated liver enzymes, or cholangitis. Bleeding is an uncommon complication that may occur from stent impaction, with the duodenal wall as the most common site with treatment being endoscopic removal. There have been few cases reported of stent migration to the colon. To our knowledge, this is the first reported case of a metal stent migration to the rectum, with erosion into the rectal wall resulting in hemorrhagic shock and perforation.

Figure: Figure 1: Metal biliary stent with penetration of the rectal mucosa.
Disclosures:
Sarah Burroughs indicated no relevant financial relationships.
Michael Sprang indicated no relevant financial relationships.
Sarah Burroughs, DO, Michael Sprang, MD. P0664 - Metal Biliary Stent Migration: An Unexpected Cause of Hemorrhagic Shock, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
