Sunday Poster Session
Category: GI Bleeding
P0669 - An Unusual Cause of Upper GI Bleeding: Mesh Perforation of the Esophagus Two Years After Hiatal Hernia Repair
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Chase H. Warashina, MD
University of Hawaii
Honolulu, HI
Presenting Author(s)
Chase Warashina, MD1, Landon Kozai, MD2, Kevin Edward Nebrejas, MD1, Traci T. Murakami, MD3
1University of Hawaii, Honolulu, HI; 2University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 3Queen's Medical Center - West Oahu, Ewa Beach, HI
Introduction: A patient with alcohol use disorder presenting with acute intoxication may present with an upper GI bleed due to gastritis or a Mallory-Weiss tear . Often, the bleeding resolves as the impetus is treated. Mesh-related complications following hiatal hernia repair remain relatively infrequent. Literature primarily reports mesh migration into the stomach. This report discusses an unusual complication: mesh perforation into the GE junction of the esophagus.
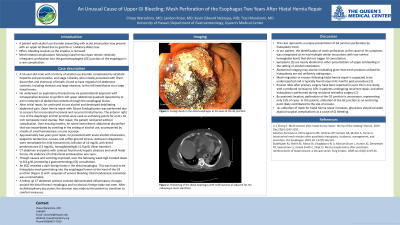
Case Description/Methods: A 55-year-old male with a history of alcohol use disorder complicated by alcoholic hepatitis and pancreatitis, obesity, and hiatal hernia repair two years prior with composite mesh overlay presents with acute alcohol intoxication, epigastric tenderness, nausea, and coffee-ground emesis. Labs were remarkable for mild transaminitis, bilirubin of 16 mg/dL with direct predominance (13 mg/dL). Hemoglobin on admission was 11.8 g/dL, but subsequently trended down to 8.8 g/dL over the following week, prompting a gastroenterology consultation. Initial CT abdomen and pelvis with contrast found only hepatic steatosis and small hiatal hernia. An EGD revealed a dark foreign body in the distal esophagus. This was found to be hiatoplasty mesh penetrating into the esophageal lumen at the level of the GE junction with sequelae of venous bleeding. EGD was unremarkable distally. A follow up CT abdomen without contrast showed inflammatory changes around the distal thoracic esophagus and no obvious foreign body was seen. After multidisciplinary discussion and given his progressive multiorgan failure (MELD 38), he was deemed a poor surgical candidate. Ultimately, the decision was made to transition to comfort measures.
Discussion: In our patient, the identification of mesh perforation as the cause of his symptoms was unexpected as he had multiple similar encounters with low-normal hemoglobin levels that did not trigger GI consultation. Mesh migration or erosion following hiatal hernia repair is suspected to be underreported, typically found around 42 months post-procedure [2]. Abdominal imaging may also be misleading given that mesh products utilized for hiatoplasty are not uniformly radiopaque. Symptoms [3] are nearly identical to other presentations of upper GI bleeding in the setting of alcohol intoxication. This case represents a unique presentation of esophageal perforation by hiatoplasty mesh presenting as GI bleeding.

Disclosures:
Chase Warashina, MD1, Landon Kozai, MD2, Kevin Edward Nebrejas, MD1, Traci T. Murakami, MD3. P0669 - An Unusual Cause of Upper GI Bleeding: Mesh Perforation of the Esophagus Two Years After Hiatal Hernia Repair, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Hawaii, Honolulu, HI; 2University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 3Queen's Medical Center - West Oahu, Ewa Beach, HI
Introduction: A patient with alcohol use disorder presenting with acute intoxication may present with an upper GI bleed due to gastritis or a Mallory-Weiss tear . Often, the bleeding resolves as the impetus is treated. Mesh-related complications following hiatal hernia repair remain relatively infrequent. Literature primarily reports mesh migration into the stomach. This report discusses an unusual complication: mesh perforation into the GE junction of the esophagus.
Case Description/Methods: A 55-year-old male with a history of alcohol use disorder complicated by alcoholic hepatitis and pancreatitis, obesity, and hiatal hernia repair two years prior with composite mesh overlay presents with acute alcohol intoxication, epigastric tenderness, nausea, and coffee-ground emesis. Labs were remarkable for mild transaminitis, bilirubin of 16 mg/dL with direct predominance (13 mg/dL). Hemoglobin on admission was 11.8 g/dL, but subsequently trended down to 8.8 g/dL over the following week, prompting a gastroenterology consultation. Initial CT abdomen and pelvis with contrast found only hepatic steatosis and small hiatal hernia. An EGD revealed a dark foreign body in the distal esophagus. This was found to be hiatoplasty mesh penetrating into the esophageal lumen at the level of the GE junction with sequelae of venous bleeding. EGD was unremarkable distally. A follow up CT abdomen without contrast showed inflammatory changes around the distal thoracic esophagus and no obvious foreign body was seen. After multidisciplinary discussion and given his progressive multiorgan failure (MELD 38), he was deemed a poor surgical candidate. Ultimately, the decision was made to transition to comfort measures.
Discussion: In our patient, the identification of mesh perforation as the cause of his symptoms was unexpected as he had multiple similar encounters with low-normal hemoglobin levels that did not trigger GI consultation. Mesh migration or erosion following hiatal hernia repair is suspected to be underreported, typically found around 42 months post-procedure [2]. Abdominal imaging may also be misleading given that mesh products utilized for hiatoplasty are not uniformly radiopaque. Symptoms [3] are nearly identical to other presentations of upper GI bleeding in the setting of alcohol intoxication. This case represents a unique presentation of esophageal perforation by hiatoplasty mesh presenting as GI bleeding.

Figure: Foreign body in the distal esophagus at the level of the GE junction.
Disclosures:
Chase Warashina indicated no relevant financial relationships.
Landon Kozai indicated no relevant financial relationships.
Kevin Edward Nebrejas indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Chase Warashina, MD1, Landon Kozai, MD2, Kevin Edward Nebrejas, MD1, Traci T. Murakami, MD3. P0669 - An Unusual Cause of Upper GI Bleeding: Mesh Perforation of the Esophagus Two Years After Hiatal Hernia Repair, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
