Sunday Poster Session
Category: GI Bleeding
P0671 - Vascular Malformations Causing GI Bleed in a Patient With Turner Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Madeline Sesselmann, DO
Advocate Aurora Health
Chicago, IL
Presenting Author(s)
Madeline Sesselmann, DO1, David H. Kruchko, DO1, Vijeta Reddy Pamudurthy, DO2
1Advocate Aurora Health, Chicago, IL; 2Advocate Aurora Health, Park Ridge, IL
Introduction: Gastrointestinal manifestations of Turner syndrome are less reported, though there have been prior cases reporting GI bleeding due to vascular malformations. We present a case of recurrent melena in a patient with Turner Syndrome with known small bowel arteriovenous malformations (AVMs).
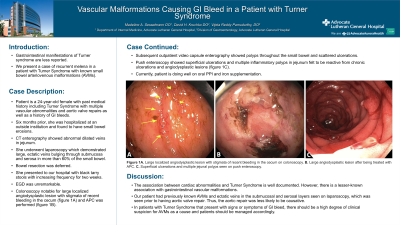
Case Description/Methods: We present a 24-year-old female with past medical history including Turner Syndrome with multiple vascular abnormalities and aortic valve repair as well as a history of GI bleeds, on oral iron supplementation. Six months prior to presentation, patient was hospitalized at an outside institution and found to have small bowel erosions. CT enterography demonstrated abnormal dilated veins in jejunum. She underwent laparoscopy which demonstrated large, ectatic veins bulging through submucosa and serosa in more than 60% of the small bowel. Due to level of involvement, bowel resection was deferred at that time. She presented to our hospital with black tarry stools with increasing frequency for two weeks. EGD was unremarkable and colonoscopy was notable for large localized angiodysplastic lesion with stigmata of recent bleeding in the cecum. APC was performed and the following day she was deemed stable for discharge. Subsequent video capsule enterography exhibited polyps throughout the small bowel and scattered ulcerations. Push enteroscopy showed superficial ulcerations and multiple jejunal polyps, with pathology findings suggesting inflammatory polyps, reactive from chronic ulcerations and angiodysplastic lesions. Currently, patient is doing well on oral proton pump inhibitor and iron supplementation.
Discussion: The association between cardiac abnormalities and Turner Syndrome is well documented, however there is a lesser-known association with gastrointestinal vascular malformations. Despite her aortic repair, she had previously known AVMs and ectatic veins in submucosal and serosal layers seen on laparoscopy, making the aortic repair less likely to be causative. In patients with Turner Syndrome that present with signs or symptoms of GI bleed, there should be a high degree of clinical suspicion for AVMs as a cause and patients should be managed accordingly.

Disclosures:
Madeline Sesselmann, DO1, David H. Kruchko, DO1, Vijeta Reddy Pamudurthy, DO2. P0671 - Vascular Malformations Causing GI Bleed in a Patient With Turner Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Advocate Aurora Health, Chicago, IL; 2Advocate Aurora Health, Park Ridge, IL
Introduction: Gastrointestinal manifestations of Turner syndrome are less reported, though there have been prior cases reporting GI bleeding due to vascular malformations. We present a case of recurrent melena in a patient with Turner Syndrome with known small bowel arteriovenous malformations (AVMs).
Case Description/Methods: We present a 24-year-old female with past medical history including Turner Syndrome with multiple vascular abnormalities and aortic valve repair as well as a history of GI bleeds, on oral iron supplementation. Six months prior to presentation, patient was hospitalized at an outside institution and found to have small bowel erosions. CT enterography demonstrated abnormal dilated veins in jejunum. She underwent laparoscopy which demonstrated large, ectatic veins bulging through submucosa and serosa in more than 60% of the small bowel. Due to level of involvement, bowel resection was deferred at that time. She presented to our hospital with black tarry stools with increasing frequency for two weeks. EGD was unremarkable and colonoscopy was notable for large localized angiodysplastic lesion with stigmata of recent bleeding in the cecum. APC was performed and the following day she was deemed stable for discharge. Subsequent video capsule enterography exhibited polyps throughout the small bowel and scattered ulcerations. Push enteroscopy showed superficial ulcerations and multiple jejunal polyps, with pathology findings suggesting inflammatory polyps, reactive from chronic ulcerations and angiodysplastic lesions. Currently, patient is doing well on oral proton pump inhibitor and iron supplementation.
Discussion: The association between cardiac abnormalities and Turner Syndrome is well documented, however there is a lesser-known association with gastrointestinal vascular malformations. Despite her aortic repair, she had previously known AVMs and ectatic veins in submucosal and serosal layers seen on laparoscopy, making the aortic repair less likely to be causative. In patients with Turner Syndrome that present with signs or symptoms of GI bleed, there should be a high degree of clinical suspicion for AVMs as a cause and patients should be managed accordingly.

Figure: Figure 1A. Large localized angiodysplastic lesion with stigmata of recent bleeding in the cecum on colonoscopy. B. Large angiodysplastic lesion after being treated with APC. C. Superficial ulcerations and multiple jejunal polyps seen on push enteroscopy.
Disclosures:
Madeline Sesselmann indicated no relevant financial relationships.
David Kruchko indicated no relevant financial relationships.
Vijeta Reddy Pamudurthy indicated no relevant financial relationships.
Madeline Sesselmann, DO1, David H. Kruchko, DO1, Vijeta Reddy Pamudurthy, DO2. P0671 - Vascular Malformations Causing GI Bleed in a Patient With Turner Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
