Sunday Poster Session
Category: IBD
P0675 - Long-Term Clinical and Endoscopic Outcomes in True North Week 52 Clinical Remitters over 3 Years of Treatment with Ozanimod: An Interim Analysis of the True North Open-Label Extension Study

Anita Afzali, MD, MPH, FACG
Executive Vice Chair of Internal Medicine, Interim Division Director of Digestive Diseases, Associate Chief Medical Officer
University of Cincinnati College of Medicine
Cincinnati, OH
Presenting Author(s)
1University of Cincinnati College of Medicine, Cincinnati, OH; 2Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL; 3University of Miami Miller School of Medicine, Miami, FL; 4Inflammatory Bowel Disease Center, Swedish Medical Center, Seattle, WA; 5Bristol Myers Squibb, Princeton, NJ; 6IRCCS San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Lombardia, Italy; 7University of Calgary, Calgary, AB, Canada
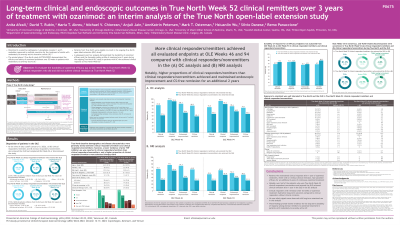
Introduction: Ozanimod (OZA), a selective sphingosine 1-phosphate receptor modulator, is approved for the treatment of moderately to severely active ulcerative colitis (UC) based on results from the phase 3 True North (TN) study, which demonstrated the efficacy and safety of OZA over 52 weeks. A subsequent post hoc analysis demonstrated the durability of OZA efficacy and favorable safety profile of OZA over 3 years during the ongoing TN OLE in patients with UC who achieved clinical response at TN Week (W) 52.
Methods: The present interim analysis of the TN OLE expands the evaluation of TN W52 clinical responders to include those who achieved clinical remission at TN W52 (ie, clinical remitters) vs those who did not (ie, clinical nonremitters) before entering the TN OLE. Clinical remission, clinical response, endoscopic improvement, and corticosteroid (CS)–free remission were evaluated in TN W52 clinical remitters vs nonremitters at OLE W46 and OLE W94 using observed case (OC) and nonresponder imputation (NRI) analyses.
Results: In all, 131 patients entered the OLE as TN W52 clinical responders on continuous OZA therapy; of these patients, 63% (83/131) were clinical remitters. All patients had received 146 weeks of continuous OZA treatment up to OLE W94 or discontinued treatment. TN baseline demographic and disease characteristics were generally similar between the 2 groups, but a lower incidence of prior tumor necrosis factor (TNF) inhibitor use was reported in clinical remitters (25.3% [21/83]) vs clinical nonremitters (43.8% [21/48]); prior non–anti-TNF biologic use was similar between groups. Compared with clinical nonremitters, more clinical remitters achieved the evaluated efficacy endpoints at OLE W46 and OLE W94 in the OC analysis (Table). A similar trend was observed in the NRI analysis. Durability of response for all efficacy endpoints was sustained from OLE W46 to OLE W94 in most clinical remitters and nonremitters, respectively: 68.5% (37/54) and 75.0% (12/16); clinical response: 75.0% (48/64) and 75.9% (22/29); endoscopic improvement: 66.1% (41/62) and 68.4% (13/19); and CS-free remission: 67.9% (36/53) and 80.0% (12/15).
Discussion: Most patients who achieved clinical remission after 1 year of OZA had sustained efficacy for an additional 2 years of continuous OZA treatment. These findings provide further evidence for the long-term durability of OZA treatment in patients with moderately to severely active UC.
| Clinical remitters at TN W52 (n=83) | Clinical nonremitters at TN W52 (n=48) | ||
OLE W46 | OLE W94 | OLE W46 | OLE W94 | |
Clinical remission,a % (n/N) | 97.0 (64/66) | 94.4 (51/54) | 93.5 (29/31) | 85.2 (23/27) |
Clinical response,b % (n/N) | 81.8 (54/66) | 75.9 (41/54) | 51.6 (16/31) | 55.6 (15/27) |
Endoscopic improvement,c % (n/N) | 86.1 (62/72) | 78.6 (44/56) | 59.4 (19/32) | 63.3 (19/30) |
CS-free remission,d % (n/N) | 80.3 (53/66) | 74.1 (40/54) | 48.4 (15/31) | 55.6 (15/27) |
Table. OZA efficacy at OLE W46 and OLE W94 in TN W52 clinical responders with or without clinical remission (OC analysis).
Note: Denominators for the OC analyses were based on the numbers of patients who completed OLE W46 or OLE W94 and had data available for the endpoints in question. aClinical remission: RBS=0 point and SFS ≤1 point, a decrease of ≥1 point from the baseline SFS, and endoscopy subscore ≤1 point. bClinical response: reduction from baseline in the 9-point Mayo score (sum of the RBS, SFS, and endoscopy subscore) of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of ≤1 point. cEndoscopic improvement: endoscopy subscore of ≤1. dCS-free remission: clinical remission while off CS for ≥12 weeks.
RBS, rectal bleeding subscore; SFS, stool frequency subscore.
Disclosures:
Anita Afzali, MD, MPH, FACG1, David T. Rubin, MD2, Maria T. Abreu, MD3, Michael V.. Chiorean, MD4, Lucy Akukwe, PharmD, MS5, Anjali Jain, PhD5, AnnKatrin Petersen, MD5, Mark T. Osterman, MD, PhD5, Hsiuanlin Wu, MS5, Silvio Danese, MD, PhD6, Remo Panaccione, MD7. P0675 - Long-Term Clinical and Endoscopic Outcomes in True North Week 52 Clinical Remitters over 3 Years of Treatment with Ozanimod: An Interim Analysis of the True North Open-Label Extension Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

