Sunday Poster Session
Category: IBD
P0682 - Effectiveness and Safety of Dual Targeted Therapy for Partially or Non-Responsive Inflammatory Bowel Disease: A Meta-Analysis and Systemic Review
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Elliot Berinstein, MD, MSc
Trinity Health Ann Arbor
Ypsilanti, MI
Presenting Author(s)
Elliot Berinstein, MD, MSc1, Shirley Cohen-Mekelburg, MD, MS2, Shrinivas Bishu, MD, PhD2, Peter Higgins, MD, PhD, MSc3, Jeffrey Berinstein, MD, MSc3
1Trinity Health Ann Arbor, Ypsilanti, MI; 2University of Michigan, Ann Arbor, MI; 3University of Michigan Hospital, Ann Arbor, MI
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition associated with a high symptom burden, disabling complications, and frequent need for surgery. Recent targeted monoclonal antibodies and small molecule therapies have significantly improved the ability to control IBD symptoms and minimize progression. Despite the use of targeted monotherapy, clinical remission is achieved in 30-50% of patients, highlighting the need for more effective therapeutics. The use of dual targeted therapy (DTT) (combining biologic medication and/or targeted small molecules) has emerged as a potential therapeutic option for patients with active IBD who are unable to achieve remission with biologic or small molecule monotherapy. We conducted a meta-analysis and systematic review of DTT in patients with IBD to provide information on the effectiveness and safety.
Methods: We conducted a systematic search of MEDLINE, EMBASE, Scopus, CINAHL Complete, Web of Science Core Collection, and Cochrane Library to identify articles related to the use of DTT for the treatment of Crohn Disease or ulcerative colitis published before May 2023. Studies that reported on at least 8 patients with IBD who received a combination of targeted therapies for the treatment of partially or non-responsive luminal IBD were eligible for inclusion. Pooled analyses of the percentage of patients experiencing clinical response, endoscopic response, and adverse events were calculated.
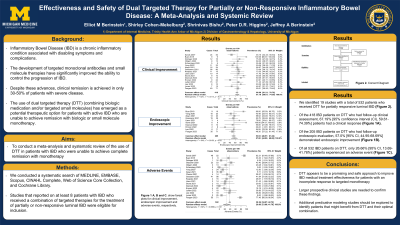
Results: We identified 19 studies with a total of 532 patients who received DTT for partially responsive luminal IBD. Of the 418 IBD patients on DTT who had follow-up clinical assessment, 67.19% [95% confidence interval (CI), 59.61-74.39%] patients had a clinical response (Figure 1A). Of the 205 IBD patients on DTT who had follow-up endoscopic evaluation, 57.0% [95% CI, 44.95-68.69%] demonstrated endoscopic improvement (Figure 1B). Of all 532 IBD patients on DTT, only 26.66% [95% CI, 13.69-41.78%] patients experienced an adverse event (Figure 1C).
Discussion: DTT appears to be a promising and safe approach to improve IBD treatment effectiveness for patients with an incomplete response to targeted monotherapy. Larger prospective clinical studies are needed to confirm these findings as is additional predictive modeling to identify the patient subgroups most likely to require and benefit from this approach.

Disclosures:
Elliot Berinstein, MD, MSc1, Shirley Cohen-Mekelburg, MD, MS2, Shrinivas Bishu, MD, PhD2, Peter Higgins, MD, PhD, MSc3, Jeffrey Berinstein, MD, MSc3. P0682 - Effectiveness and Safety of Dual Targeted Therapy for Partially or Non-Responsive Inflammatory Bowel Disease: A Meta-Analysis and Systemic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Trinity Health Ann Arbor, Ypsilanti, MI; 2University of Michigan, Ann Arbor, MI; 3University of Michigan Hospital, Ann Arbor, MI
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition associated with a high symptom burden, disabling complications, and frequent need for surgery. Recent targeted monoclonal antibodies and small molecule therapies have significantly improved the ability to control IBD symptoms and minimize progression. Despite the use of targeted monotherapy, clinical remission is achieved in 30-50% of patients, highlighting the need for more effective therapeutics. The use of dual targeted therapy (DTT) (combining biologic medication and/or targeted small molecules) has emerged as a potential therapeutic option for patients with active IBD who are unable to achieve remission with biologic or small molecule monotherapy. We conducted a meta-analysis and systematic review of DTT in patients with IBD to provide information on the effectiveness and safety.
Methods: We conducted a systematic search of MEDLINE, EMBASE, Scopus, CINAHL Complete, Web of Science Core Collection, and Cochrane Library to identify articles related to the use of DTT for the treatment of Crohn Disease or ulcerative colitis published before May 2023. Studies that reported on at least 8 patients with IBD who received a combination of targeted therapies for the treatment of partially or non-responsive luminal IBD were eligible for inclusion. Pooled analyses of the percentage of patients experiencing clinical response, endoscopic response, and adverse events were calculated.
Results: We identified 19 studies with a total of 532 patients who received DTT for partially responsive luminal IBD. Of the 418 IBD patients on DTT who had follow-up clinical assessment, 67.19% [95% confidence interval (CI), 59.61-74.39%] patients had a clinical response (Figure 1A). Of the 205 IBD patients on DTT who had follow-up endoscopic evaluation, 57.0% [95% CI, 44.95-68.69%] demonstrated endoscopic improvement (Figure 1B). Of all 532 IBD patients on DTT, only 26.66% [95% CI, 13.69-41.78%] patients experienced an adverse event (Figure 1C).
Discussion: DTT appears to be a promising and safe approach to improve IBD treatment effectiveness for patients with an incomplete response to targeted monotherapy. Larger prospective clinical studies are needed to confirm these findings as is additional predictive modeling to identify the patient subgroups most likely to require and benefit from this approach.

Figure: Figure 1A shows a forest plot of all patients who had clinical assessment before and after initiation of DTT. Figure 1B shows a forest plot of all patients who had endoscopic assessment before and after initiation of DTT. Figure 1C shows a forest plot of adverse events of patients on DTT
Disclosures:
Elliot Berinstein indicated no relevant financial relationships.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Shrinivas Bishu indicated no relevant financial relationships.
Peter Higgins: AbbVie – Consultant. Amgen – Consultant. Buhlmann Laboratories – Consultant. Celltrion – Consultant. Curacle – Consultant. Eli Lilly – Consultant. Genentech – Consultant.
Jeffrey Berinstein: Bristol Myers Squibb – Consultant. Buhlman Diagnostics – Consultant. Oshi Health – Consultant.
Elliot Berinstein, MD, MSc1, Shirley Cohen-Mekelburg, MD, MS2, Shrinivas Bishu, MD, PhD2, Peter Higgins, MD, PhD, MSc3, Jeffrey Berinstein, MD, MSc3. P0682 - Effectiveness and Safety of Dual Targeted Therapy for Partially or Non-Responsive Inflammatory Bowel Disease: A Meta-Analysis and Systemic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

