Sunday Poster Session
Category: IBD
P0708 - Factors Associated With Crohn’s Disease Progression Events in the IBD PLEXUS and IQVIA Linked Dataset
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- MS
Mirko Sikirica, PharmD
Janssen Immunology
Horsham, Pennsylvania
Presenting Author(s)
Mirko Sikirica, PharmD1, Matt Molaei, PharmD, MS1, Ravi Patel, PharmD, MS1, Kirsten Lum, PhD, MS2
1Janssen Immunology, Horsham, PA; 2Janssen Data Science, Raritan, NJ
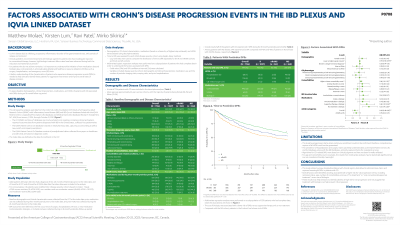
Introduction: Crohn’s disease (CD) is a life-long inflammatory disorder with intermittent events indicating disease progression. However, CD studies using real-world long-term administrative claims databases do not include disease severity measures or robust clinical disease data. We evaluated baseline demographics, clinical characteristics, medications and healthcare utilization of patients (pts) with CD associated with disease progression events (DPE) during an 18-month follow-up.
Methods: This retrospective analysis used data from the Crohn’s & Colitis Foundation (CCF) SPARC IBD and IBD QORUS data linked with IQVIA’s prescription and medical claims, to identify a cohort of CD pts with up to 24 months pre-enrollment and at least 18 months of follow-up. Enrollment date into CCF was used as the Index date. The DPE outcomes were collected during an 18-month post-index follow up and defined as first occurrence of: surgery, hospitalization, ER visit, new medication (Corticosteroids, Biologics or 5ASAs). Demographics, CD clinical characteristics, medication (based on a hierarchy of highest step achieved), and healthcare resource utilization were used in descriptive analyses and were used (as available) in multivariable logistic regression analyses predicting factors associated with DPE.
Results: 1756 CD pts were identified for baseline descriptive analyses. Pts mean age was 43.0 yrs old, 58.4% female, 87% non-Hispanic, 75% white. Time since diagnosis 14.6yrs, mean (±SD) sCDAI scores at enrollment 157 (±92.3). Biologics were used by 37.0% of pts, conventional/supportive medications were used by 49.9%, and 21.8% were not on any treatment for CD (Table 1). Multivariable analyses were run on 1278 patients which had complete data. Remitters (sCDAI< 150) were at lower risk of DPE [OR: 0.65, 95% CI (0.48–0.88)] compared to Moderate-Severe (sCDAI >220). As well, a lower age [OR: 0.99, 95% CI (0.98–0.99)], higher number of comorbidities [OR: 1.07, 95% CI (1.01–1.15)], and use of No Treatment [OR: 1.64, 95% CI (1.19–2.25)] or only conventional/supportive treatment [OR: 1.48, 95% CI (1.07–2.04)] were statistically significantly associated with higher DPE.
Discussion: We utilized a longitudinal dataset linked to administrative claims to capture meaningful CD DPE. We identified several factors including: Remission status, age, number of comorbidities and use of 'no treatment’ or ‘only conventional/supportive treatment’ versus biologics were associated with higher risk for CD progression events.
Disclosures:
Mirko Sikirica, PharmD1, Matt Molaei, PharmD, MS1, Ravi Patel, PharmD, MS1, Kirsten Lum, PhD, MS2. P0708 - Factors Associated With Crohn’s Disease Progression Events in the IBD PLEXUS and IQVIA Linked Dataset, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Janssen Immunology, Horsham, PA; 2Janssen Data Science, Raritan, NJ
Introduction: Crohn’s disease (CD) is a life-long inflammatory disorder with intermittent events indicating disease progression. However, CD studies using real-world long-term administrative claims databases do not include disease severity measures or robust clinical disease data. We evaluated baseline demographics, clinical characteristics, medications and healthcare utilization of patients (pts) with CD associated with disease progression events (DPE) during an 18-month follow-up.
Methods: This retrospective analysis used data from the Crohn’s & Colitis Foundation (CCF) SPARC IBD and IBD QORUS data linked with IQVIA’s prescription and medical claims, to identify a cohort of CD pts with up to 24 months pre-enrollment and at least 18 months of follow-up. Enrollment date into CCF was used as the Index date. The DPE outcomes were collected during an 18-month post-index follow up and defined as first occurrence of: surgery, hospitalization, ER visit, new medication (Corticosteroids, Biologics or 5ASAs). Demographics, CD clinical characteristics, medication (based on a hierarchy of highest step achieved), and healthcare resource utilization were used in descriptive analyses and were used (as available) in multivariable logistic regression analyses predicting factors associated with DPE.
Results: 1756 CD pts were identified for baseline descriptive analyses. Pts mean age was 43.0 yrs old, 58.4% female, 87% non-Hispanic, 75% white. Time since diagnosis 14.6yrs, mean (±SD) sCDAI scores at enrollment 157 (±92.3). Biologics were used by 37.0% of pts, conventional/supportive medications were used by 49.9%, and 21.8% were not on any treatment for CD (Table 1). Multivariable analyses were run on 1278 patients which had complete data. Remitters (sCDAI< 150) were at lower risk of DPE [OR: 0.65, 95% CI (0.48–0.88)] compared to Moderate-Severe (sCDAI >220). As well, a lower age [OR: 0.99, 95% CI (0.98–0.99)], higher number of comorbidities [OR: 1.07, 95% CI (1.01–1.15)], and use of No Treatment [OR: 1.64, 95% CI (1.19–2.25)] or only conventional/supportive treatment [OR: 1.48, 95% CI (1.07–2.04)] were statistically significantly associated with higher DPE.
Discussion: We utilized a longitudinal dataset linked to administrative claims to capture meaningful CD DPE. We identified several factors including: Remission status, age, number of comorbidities and use of 'no treatment’ or ‘only conventional/supportive treatment’ versus biologics were associated with higher risk for CD progression events.
Table: Table 1: Demographics, Disease Characteristics, Medications and Healthcare Utilization
Disclosures:
Mirko Sikirica: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Matt Molaei: Johnson & Johnson – Employee, Stock-publicly held company(excluding mutual/index funds).
Ravi Patel: Johnson & Johnson – Employee, Post-Doctorate Fellow at Janssen Immunology at time of study.
Kirsten Lum: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Mirko Sikirica, PharmD1, Matt Molaei, PharmD, MS1, Ravi Patel, PharmD, MS1, Kirsten Lum, PhD, MS2. P0708 - Factors Associated With Crohn’s Disease Progression Events in the IBD PLEXUS and IQVIA Linked Dataset, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
