Sunday Poster Session
Category: IBD
P0722 - Predictors of Major Adverse Cardiac and Cerebrovascular Events in Inflammatory Bowel Disease Using Artificial Neural Network Analysis in a Nationally Representative US Cohort
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aleen Rahman, MBBS
Fatima Jinnah Medical University
San Jose, CA
Presenting Author(s)
Aleen Rahman, MBBS1, Nigil Thaimuriyil, DO2, Medha Rajamanuri, MD3, Bhavi Trivedi, MBBS4, Dhruvi Modi, MBBS5, Borzoo Tajdin, MD6, Vikash Kumar, MD7, Revanth Reddy, MD8, Yashwitha Sai Pulakurthi, MBBS9, Rupak Desai, MBBS10, Rewanth Katamreddy, MD11
1Fatima Jinnah Medical University, San Jose, CA; 2Baptist Hospitals of Southeast Texas, Newark, NJ; 3Charleston Area Medical Center, Charleston, WV; 4Texas Tech University Health Sciences Center, El Paso, TX; 5Gujrat Adani Institute of Medical Sciences, Gujrat, Gujarat, India; 6Shahid Beheshti University of Medical Sciences, Tehran, Tehran, Iran; 7Brooklyn Hospital Center, Brooklyn, NY; 8East Carolina University, Greenville, NC; 9New York Medical College-Saint Michael's Medical Center, Newark, NJ; 10Outcomes Research, Atlanta, GA; 11Saint Michael’s Medical Center, Newark, NJ
Introduction: Inflammatory Bowel Disease (IBD) patients have a higher risk of cardio and cerebrovascular adverse events, causing an increased all-cause in-hospital mortality (ACM), length of stay, & resource utilization during in-hospital care due to comorbid disorders.
Methods: Using the 2019 National Inpatient Sample, we analyzed IBD hospitalizations with comorbidities. Artificial Neural Network (ANN) predictive factors were selected. We randomly split patients with IBD-related hospitalizations (unweighted n=63,724) into training data (n=44,768, 70%) & testing data (n=18,956, 30%). The training data calibrated the ANN, while the testing data evaluated the algorithm's accuracy. We compared incorrect prediction frequencies between the two datasets and measured the area under the Receiver Operating Curve (AUC) to assess the ANN's efficacy in predicting clinical outcomes, including major adverse cardiac and cerebrovascular events (MACCE), all-cause in-hospital mortality (ACM), acute myocardial infarction (AMI), cardiac arrest (CA), & stroke.
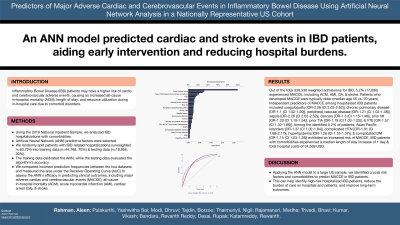
Results: Out of the total 330,530 weighted admissions for IBD, 5.2% (17,090) experienced MACCE, including ACM, AMI, CA, & stroke. Patients who developed MACCE were typically older (median age 55 vs.70 years), Medicare enrollees (65.7% vs. 42.3%), & admitted non-electively (94.6% vs. 83.9%). Independent predictors of MACCE among hospitalized IBD patients included coagulopathy [OR-2.26 (CI 2.02-2.52)], chronic pulmonary disease [OR-1.1 (CI 1.02-1.20)], peripheral vascular disease [OR-1.21 (CI 1.02-1.38)], sepsis [OR-2.26 (CI 2.02-2.52)], cancers [OR-1.3 (CI 1.15-1.46)], prior MI [OR-1.33 (CI 1.15-1.54)], prior TIA [OR-1.19 (CI 1.03-1.33)], & VTE [OR-1.57 (CI 1.32-1.86)]. Among the identified 5.2% of patients, Asian Pacific Islanders [OR-1.37 (CI 1.02-1.84)], complicated HTN [OR-1.91 (CI 1.68-2.17)], hyperlipidemia [OR-1.26 (CI 1.16-1.37)], & complicated DM [OR-1.15 (CI 1.03-1.28)] exhibited an increased risk of MACCE. IBD patients with comorbidities experienced a median length of stay increase of 1 day & total hospital costs of 34,569 USD. All p-values were < 0.001. Normalized predictors are shown in Figure 1a, & the AUC in Figure 1b is 0.776, indicating an acceptable prediction model.
Discussion: Applying the ANN model to a large US sample, we identified crucial risk factors and comorbidities to predict MACCE in IBD patients. This can help identify high-risk hospitalized IBD patients, reduce the burden of care on hospitals and patients, and improve long-term outcomes.

Disclosures:
Aleen Rahman, MBBS1, Nigil Thaimuriyil, DO2, Medha Rajamanuri, MD3, Bhavi Trivedi, MBBS4, Dhruvi Modi, MBBS5, Borzoo Tajdin, MD6, Vikash Kumar, MD7, Revanth Reddy, MD8, Yashwitha Sai Pulakurthi, MBBS9, Rupak Desai, MBBS10, Rewanth Katamreddy, MD11. P0722 - Predictors of Major Adverse Cardiac and Cerebrovascular Events in Inflammatory Bowel Disease Using Artificial Neural Network Analysis in a Nationally Representative US Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Fatima Jinnah Medical University, San Jose, CA; 2Baptist Hospitals of Southeast Texas, Newark, NJ; 3Charleston Area Medical Center, Charleston, WV; 4Texas Tech University Health Sciences Center, El Paso, TX; 5Gujrat Adani Institute of Medical Sciences, Gujrat, Gujarat, India; 6Shahid Beheshti University of Medical Sciences, Tehran, Tehran, Iran; 7Brooklyn Hospital Center, Brooklyn, NY; 8East Carolina University, Greenville, NC; 9New York Medical College-Saint Michael's Medical Center, Newark, NJ; 10Outcomes Research, Atlanta, GA; 11Saint Michael’s Medical Center, Newark, NJ
Introduction: Inflammatory Bowel Disease (IBD) patients have a higher risk of cardio and cerebrovascular adverse events, causing an increased all-cause in-hospital mortality (ACM), length of stay, & resource utilization during in-hospital care due to comorbid disorders.
Methods: Using the 2019 National Inpatient Sample, we analyzed IBD hospitalizations with comorbidities. Artificial Neural Network (ANN) predictive factors were selected. We randomly split patients with IBD-related hospitalizations (unweighted n=63,724) into training data (n=44,768, 70%) & testing data (n=18,956, 30%). The training data calibrated the ANN, while the testing data evaluated the algorithm's accuracy. We compared incorrect prediction frequencies between the two datasets and measured the area under the Receiver Operating Curve (AUC) to assess the ANN's efficacy in predicting clinical outcomes, including major adverse cardiac and cerebrovascular events (MACCE), all-cause in-hospital mortality (ACM), acute myocardial infarction (AMI), cardiac arrest (CA), & stroke.
Results: Out of the total 330,530 weighted admissions for IBD, 5.2% (17,090) experienced MACCE, including ACM, AMI, CA, & stroke. Patients who developed MACCE were typically older (median age 55 vs.70 years), Medicare enrollees (65.7% vs. 42.3%), & admitted non-electively (94.6% vs. 83.9%). Independent predictors of MACCE among hospitalized IBD patients included coagulopathy [OR-2.26 (CI 2.02-2.52)], chronic pulmonary disease [OR-1.1 (CI 1.02-1.20)], peripheral vascular disease [OR-1.21 (CI 1.02-1.38)], sepsis [OR-2.26 (CI 2.02-2.52)], cancers [OR-1.3 (CI 1.15-1.46)], prior MI [OR-1.33 (CI 1.15-1.54)], prior TIA [OR-1.19 (CI 1.03-1.33)], & VTE [OR-1.57 (CI 1.32-1.86)]. Among the identified 5.2% of patients, Asian Pacific Islanders [OR-1.37 (CI 1.02-1.84)], complicated HTN [OR-1.91 (CI 1.68-2.17)], hyperlipidemia [OR-1.26 (CI 1.16-1.37)], & complicated DM [OR-1.15 (CI 1.03-1.28)] exhibited an increased risk of MACCE. IBD patients with comorbidities experienced a median length of stay increase of 1 day & total hospital costs of 34,569 USD. All p-values were < 0.001. Normalized predictors are shown in Figure 1a, & the AUC in Figure 1b is 0.776, indicating an acceptable prediction model.
Discussion: Applying the ANN model to a large US sample, we identified crucial risk factors and comorbidities to predict MACCE in IBD patients. This can help identify high-risk hospitalized IBD patients, reduce the burden of care on hospitals and patients, and improve long-term outcomes.

Figure: Fig.1a.shows the normalised importance of MACCE predictors in Patinets hospitalized with IBD
Fig.1b. Area under the curve for method used
Fig.1b. Area under the curve for method used
Disclosures:
Aleen Rahman indicated no relevant financial relationships.
Nigil Thaimuriyil indicated no relevant financial relationships.
Medha Rajamanuri indicated no relevant financial relationships.
Bhavi Trivedi indicated no relevant financial relationships.
Dhruvi Modi indicated no relevant financial relationships.
Borzoo Tajdin indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Revanth Reddy indicated no relevant financial relationships.
Yashwitha Sai Pulakurthi indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Aleen Rahman, MBBS1, Nigil Thaimuriyil, DO2, Medha Rajamanuri, MD3, Bhavi Trivedi, MBBS4, Dhruvi Modi, MBBS5, Borzoo Tajdin, MD6, Vikash Kumar, MD7, Revanth Reddy, MD8, Yashwitha Sai Pulakurthi, MBBS9, Rupak Desai, MBBS10, Rewanth Katamreddy, MD11. P0722 - Predictors of Major Adverse Cardiac and Cerebrovascular Events in Inflammatory Bowel Disease Using Artificial Neural Network Analysis in a Nationally Representative US Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
