Sunday Poster Session
Category: IBD
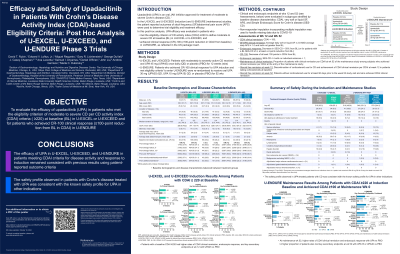
P0732 - Efficacy of Upadacitinib in Patients With Crohn’s Disease Activity Index-Based Eligibility Criteria: Post Hoc Analysis of U-EXCEL, U-EXCEED, and U-ENDURE Phase 3 Trials
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
David Rubin, MD, FACG
University of Chicago Medicine, Inflammatory Bowel Disease Center
Chicago, IL
Presenting Author(s)
David T. Rubin, MD, FACG1, Edward V.. Loftus, MD2, Miguel Regueiro, MD3, Gary Lichtenstein, MD4, Aaron DuVall, MD5, J. Casey Chapman, MD6, Ana P.. Lacerda, MD, MSc7, Samuel I.. Anyanwu, PhD, MS7, Daniel O’Brien, PhD8, Jianzhong Liu, MD, MS7, Andrew Garrison, MS7, Marla C.. Dubinsky, MD9
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2Mayo Clinic College of Medicine and Science, Rochester, MN; 3Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 4Perelman School of Medicine of the University of Pennsylvania, Philadelphia, PA; 5Tyler Research Institute, LLC, Tyler, TX; 6Louisiana State University Health Sciences Center, Crohn's and Colitis Center at the Baton Rouge General, GI Alliance, Baton Rouge, LA; 7AbbVie Inc., North Chicago, IL; 8AbbVie, North Chicago, IL; 9Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Upadacitinib (UPA) is an oral JAK inhibitor approved for treatment of moderate to severe Crohn’s disease (CD).1 In the U-EXCEL and U-EXCEED (induction) and U-ENDURE (maintenance) studies, the patient reported outcomes (PROs) of stool frequency (SF)/abdominal pain score (APS) were used to determine trial eligibility and treatment efficacy (criteria in Table footnotes). Here, UPA efficacy was evaluated in patients (pts) who met the eligibility criterion of CD activity index (CDAI; an 8-item composite index, which includes PROs) ≥220 to define moderate to severe CD at baseline (BL) in U-EXCEL or U-EXCEED and who achieved CR-100 clinical response (≥100-point reduction from BL in CDAI) in U-ENDURE, as reflected in the US package insert.
Methods: This post hoc analysis included 857 pts from U-EXCEL and U-EXCEED with BL CDAI ≥220 who received 12 weeks (wks) of UPA 45 mg (UPA45) or placebo (PBO) daily, and 343 pts from U-ENDURE who achieved CR-100 to UPA45 and were re-randomized to receive UPA 15 mg (UPA15), 30 mg (UPA30) or PBO daily. Clinical and endoscopic outcomes were assessed (see Table for endpoints). Missing data were handled as described (Table footnote). Nominal P values are presented.
Results: Pts with a BL CDAI ≥220 had higher rates of CDAI clinical remission (U-EXCEL, 46.2% vs 22.5%; U-EXCEED, 35.9% vs 17.8%), endoscopic response (U-EXCEL, 45.5% vs 12.6%; U-EXCEED, 34.1% vs 3.4%; P< 0.0001 both comparisons), and key secondary endpoints at wk 12 with UPA45 vs PBO (Table). At maintenance wk 52, higher rates of CDAI clinical remission (41.6% [UPA15], 54.6% [UPA30] vs 14.4% [PBO]) and endoscopic response (27.8% [UPA15], 41.2% [UPA30] vs 7.2% [PBO]) (P< 0.0001 for all comparisons) with UPA vs PBO. A higher proportion of pts also met key secondary endpoints (SF/APS clinical remission, CR-100, maintenance of CDAI clinical remission, steroid-free CDAI clinical remission, steroid-free CDAI clinical remission,, endoscopic remission, and CDAI clinical remission + endoscopic remission) at wk 52 with UPA15 or UPA30 vs PBO. Adverse event rates were similar across treatment groups (Table).
Discussion: The efficacy of UPA in U-EXCEL, U-EXCEED, and U-ENDURE in pts meeting CDAI criteria for disease activity and response to induction remained consistent with previous results using PRO criteria.1 No new safety signals were observed.
Disclosures:
David T. Rubin, MD, FACG1, Edward V.. Loftus, MD2, Miguel Regueiro, MD3, Gary Lichtenstein, MD4, Aaron DuVall, MD5, J. Casey Chapman, MD6, Ana P.. Lacerda, MD, MSc7, Samuel I.. Anyanwu, PhD, MS7, Daniel O’Brien, PhD8, Jianzhong Liu, MD, MS7, Andrew Garrison, MS7, Marla C.. Dubinsky, MD9. P0732 - Efficacy of Upadacitinib in Patients With Crohn’s Disease Activity Index-Based Eligibility Criteria: Post Hoc Analysis of U-EXCEL, U-EXCEED, and U-ENDURE Phase 3 Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2Mayo Clinic College of Medicine and Science, Rochester, MN; 3Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 4Perelman School of Medicine of the University of Pennsylvania, Philadelphia, PA; 5Tyler Research Institute, LLC, Tyler, TX; 6Louisiana State University Health Sciences Center, Crohn's and Colitis Center at the Baton Rouge General, GI Alliance, Baton Rouge, LA; 7AbbVie Inc., North Chicago, IL; 8AbbVie, North Chicago, IL; 9Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Upadacitinib (UPA) is an oral JAK inhibitor approved for treatment of moderate to severe Crohn’s disease (CD).1 In the U-EXCEL and U-EXCEED (induction) and U-ENDURE (maintenance) studies, the patient reported outcomes (PROs) of stool frequency (SF)/abdominal pain score (APS) were used to determine trial eligibility and treatment efficacy (criteria in Table footnotes). Here, UPA efficacy was evaluated in patients (pts) who met the eligibility criterion of CD activity index (CDAI; an 8-item composite index, which includes PROs) ≥220 to define moderate to severe CD at baseline (BL) in U-EXCEL or U-EXCEED and who achieved CR-100 clinical response (≥100-point reduction from BL in CDAI) in U-ENDURE, as reflected in the US package insert.
Methods: This post hoc analysis included 857 pts from U-EXCEL and U-EXCEED with BL CDAI ≥220 who received 12 weeks (wks) of UPA 45 mg (UPA45) or placebo (PBO) daily, and 343 pts from U-ENDURE who achieved CR-100 to UPA45 and were re-randomized to receive UPA 15 mg (UPA15), 30 mg (UPA30) or PBO daily. Clinical and endoscopic outcomes were assessed (see Table for endpoints). Missing data were handled as described (Table footnote). Nominal P values are presented.
Results: Pts with a BL CDAI ≥220 had higher rates of CDAI clinical remission (U-EXCEL, 46.2% vs 22.5%; U-EXCEED, 35.9% vs 17.8%), endoscopic response (U-EXCEL, 45.5% vs 12.6%; U-EXCEED, 34.1% vs 3.4%; P< 0.0001 both comparisons), and key secondary endpoints at wk 12 with UPA45 vs PBO (Table). At maintenance wk 52, higher rates of CDAI clinical remission (41.6% [UPA15], 54.6% [UPA30] vs 14.4% [PBO]) and endoscopic response (27.8% [UPA15], 41.2% [UPA30] vs 7.2% [PBO]) (P< 0.0001 for all comparisons) with UPA vs PBO. A higher proportion of pts also met key secondary endpoints (SF/APS clinical remission, CR-100, maintenance of CDAI clinical remission, steroid-free CDAI clinical remission, steroid-free CDAI clinical remission,, endoscopic remission, and CDAI clinical remission + endoscopic remission) at wk 52 with UPA15 or UPA30 vs PBO. Adverse event rates were similar across treatment groups (Table).
Discussion: The efficacy of UPA in U-EXCEL, U-EXCEED, and U-ENDURE in pts meeting CDAI criteria for disease activity and response to induction remained consistent with previous results using PRO criteria.1 No new safety signals were observed.
| A) U-EXCEL and U-EXCEED Induction Results Among Patients with CDAI ≥220 at Baseline | ||||||
| U-EXCEL (M14-433) | U-EXCEED (M14-431) | |||||
| PBO N=143 % [95% CI] | UPA45 N=295 % [95% CI] | Difference vs PBO % [95% CI] P-value | PBO N=146 % [95% CI] | UPA45 N=273 % [95% CI] | Difference vs PBO % [95% CI] P-value | |
| Co-primary Endpoints CDAI Clinical Remission at Wk12 Endoscopic Response at Wk12 | 22.5 [15.6, 29.4] 12.6 [7.2, 18.0] | 46.2 [40.5, 51.9] 45.5 [39.9, 51.2] | 23.8 [15.3, 32.2] P< 0.0001 33.2 [25.7, 40.6] P< 0.0001 | 17.8 [11.6, 24.0] 3.4 [0.5, 6.4] | 35.9 [30.2, 41.6] 34.1 [28.5, 39.7] | 17.3 [9.2, 25.4] P< 0.0001 29.9 [23.7, 36.1] P< 0.0001 |
| Key Secondary Endpoints SF/APS Clinical Remission at Wk12 CR-100 at Wk2 CR-100 at Wk12 Clinical Remission at Wk 4 Steroid-free Clinical Remission at Wk12 in Patients Taking Steroids at BL Endoscopic Remission at Wk12 | 20.3 [13.7, 26.9] 23.8 [16.7, 30.8] 40.3 [32.2, 48.4] 19.6 [13.1, 26.1] 13.1 [4.0, 22.1] (N=54) 7.7 [3.3, 12.1] | 52.1 [46.4, 57.8] 36.8 [31.3, 42.3] 63.8 [58.3, 69.3] 31.9 [26.6, 37.2] 39.8 [30.6, 49.0] (N=108) 30.2 [25.0, 35.5] | 31.5 [23.3, 39.8] P< 0.0001 12.9 [4.3, 21.4] P=0.0033 23.9 [14.6, 33.1] P< 0.0001 12.5 [4.7, 20.4] P=0.0018 26.5 [13.9, 39.0] P< 0.0001 22.3 [15.7, 29.0] P< 0.0001 | 14.4 [8.7, 20.1] 13.8 [8.2, 19.4] 30.8 [23.3, 38.3] 12.5 [7.1, 17.9] 11.3 [2.8, 19.9] (N=53) 3.4 [0.5, 6.4] | 39.2 [33.4, 45.0] 36.8 [31.1, 42.5] 53.8 [47.9, 59.8] 24.9 [19.8, 30.0] 30.2 [21.0, 39.4] (N=96) 18.7 [14.1, 23.3] | 24.2 [16.6, 31.8] P< 0.0001 22.4 [14.6, 30.1] P< 0.0001 22.3 [13.3, 31.3] P< 0.0001 11.9 [4.7, 19.1] P=0.0012 17.1 [5.5, 28.8] P=0.0040 15.1 [9.6, 20.5] P< 0.0001 |
| Treatment Emergent Adverse Events (TEAEs), N (%) Serious Adverse Events, N (%) TEAEs leading to discontinuation, N (%) Deaths, N (%) | 89 (62.2) 12 (8.4) 10 (7.0) 0 | 184 (62.4) 22 (7.5) 14 (4.7) 0 | 0ꓸ1 [-9.5, 9.8] -0.9 [-6.4, 4.5] -2.2 [-7.1, 2.6] 0 | 94 (64.4) 16 (11.0) 6 (4.1) 0 | 183 (67.0) 26 (9.5) 13 (4.8) 1 (0.4) | 2.6 [-6.9, 12.2] -1.4 [-7.6, 4.7] 0.7 [-3.4, 4.7] 0.4 [-0.4, 1.1] |
| B) U-ENDURE Maintenance Results Among Patients with CDAI ≥220 at Induction Baseline and Achieved CDAI ≥100 at Maintenance Wk 0 | ||||||
| PBO N=111 % [95% CI] | UPA15 N=113 % [95% CI] | Difference vs PBO % [95% CI] P-value | UPA30 N=119 % [95% CI] | Difference vs PBO % [95% CI] P-value | ||
| Co-primary Endpoints CDAI Clinical Remission at Wk52 Endoscopic Response at Wk52 | 14.4 [7.9, 20.9] 7.2 [2.4, 12.0] | 41.6 [32.5, 50.7] 27.8 [19.5, 36.2] | 28.8 [18.5, 39.1] P< 0.0001 22.4 [13.1, 31.7] P< 0.0001 | 54.6 [45.7, 63.6] 41.2 [32.3, 50.0] | 39.7 [28.8, 50.5] P< 0.0001 34.4 [24.8, 44.1] P< 0.0001 | |
| Key Secondary Endpoints SF/APS Clinical Remission at Wk52 CR-100 at Wk52 Maintenance of CDAI Clinical Remission at Wk52 Steroid-free CDAI Clinical Remission at Wk52 Steroid-free CDAI Clinical Remission at Wk52 in Patients Taking Steroids at BL Endoscopic Remission at Wk52 CDAI Clinical Remission + Endoscopic Remission at Wk52 | 15.3 [8.6, 22.0] 19.8 [12.4, 27.2] 21.9 [12.4, 31.4] (N=73) 14.4 [7.9, 20.9] 6.5 [0.0, 13.7] (N=46) 5.4 [1.2, 9.6] 3.6 [0.1, 7.1] | 38.1 [29.1, 47.0] 47.8 [38.6, 57.0] 51.4 [39.8, 62.9] (N=72) 41.6 [32.5, 50.7] 47.7 [33.0, 62.5] (N=44) 18.6 [11.4, 25.8] 16.0 [9.2, 22.7] | 24.2 [13.9, 34.4] P< 0.0001 29.5 [18.4, 40.5] P< 0.0001 32.0 [17.8, 46.1] P< 0.0001 28.8 [18.5, 39.1] P< 0.0001 42.2 [27.9, 56.6] P< 0.0001 14.2 [5.9, 22.5] P=0.0008 13.4 [5.9, 21.0] P=0.0005 | 53.8 [44.8, 62.7] 59.7 [50.8, 68.5] 67.1 [56.7, 77.5] (N=79) 52.9 [44.0, 61.9] 44.4 [29.9, 59.0] (N=45) 30.3 [22.0, 38.5] 26.1 [18.2, 33.9] | 36.7 [25.9, 47.5] P< 0.0001 38.7 [27.5, 49.9] P< 0.0001 42.8 [29.1, 56.6] P< 0.0001 38.0 [27.1, 48.9] P< 0.0001 36.4 [21.3, 51.5] P< 0.0001 24.5 [15.2, 33.8] P< 0.0001 22.4 [13.9, 31.0] P< 0.0001 | |
| Treatment Emergent Adverse Events (TEAEs), N (%) Serious Adverse Events, N (%) TEAEs leading to discontinuation, N (%) Deaths, N (%) | 86 (77.5) 16 (14.4) 4 (3.6) 0 | 86 (76.1) 14 (12.4) 9 (8.0) 0 | -1.4 [-12.4, 9.7] -2.0 [-10.9, 6.9] 4.4 [-1.7, 10.4] 0 | 96 (80.7) 13 (10.9) 8 (6.7) 0 | 3.2 [-7.3, 13.7] -3.5 [-12.1, 5.1] 3.1 [-2.6, 8.8] 0 | |
| APS, Abdominal Pain Score; BL, Baseline; CD, Crohn’s disease; CDAI, CD Activity Index; CI, Confidence Interval; CMH, Cochran-Mantel-Haenszel; CR-100, Clinical Response-100; PBO, Placebo; SF, Stool Frequency; UPA, Upadacitinib; Wk, Week. SF/APS clinical response: ≥30% decrease in average daily very soft/liquid SF and/or ≥30% decrease in average daily APS and both not worse than BL CDAI clinical remission: CDAI < 150 SF/APS clinical remission: Average daily soft or liquid SF ≤ 2.8 AND average daily APS ≤ 1.0 and both not greater than BL Endoscopic response: Decrease in SES-CD > 50% from BL (or for patients with a BL SES-CD of 4, at least a 2-point reduction from BL) CR-100: Decrease of at least 100 points in CDAI from BL Endoscopic Remission: SES-CD ≤ 4 with no individual subscore > 1 Maintenance of Clinical Remission: Proportion of patients with clinical remission per CDAI at wk 52 of the maintenance study among subjects who achieved clinical remission per CDAI at the entry of the maintenance study Steroid-free Clinical Remission: Patients without corticosteroid use for at least 90 days prior to the study visit and achieved clinical remission per CDAI Point estimate and 95% CI for treatment difference are based on CMH for categorical endpoints and MMRM for continuous endpoints. Efficacy was assessed in the intention to treat (ITT) population and included all randomized subjects in U-EXCEL and U-EXCEED who received at least one dose of study drug during induction AND had CDAI≥220 at BL; in U-ENDURE, the ITT and safety population included the first 502 randomized subjects who received at least one dose of study drug AND had CDAI≥220 at BL AND achieved CR-100 at the entry of U-ENDURE. 1. Loftus EV, Panés J, Lacerda AP, Peyrin-Biroulet L, D’Haens G, Panaccione R, et al. Upadacitinib Induction and Maintenance Therapy for Crohn’s Disease. New England Journal of Medicine. 2023 May 25;388(21):1966–80. | ||||||
Table: Table. Co-primary, Key Secondary, and Safety Endpoints
Disclosures:
David T. Rubin: AbbVie – Consultant. Alike Health – Stock Options. AltruBio – Consultant, Stock Options. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Advisory Committee/Board Member. Crohn's & Colitis Foundation – Advisory Committee/Board Member. Datos Health – Stock Options. EcoR1 – Consultant. Eli Lilly – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Iterative Health – Stock Options. Janssen – Consultant. Kaleido Biosciences – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Reistone – Consultant. Seres Therapeutics – Consultant. Syneos – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Trellus Health – Consultant.
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Alvotech – Consultant. Amgen – Consultant. Arena – Consultant. Avalo Therapeutics – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support. Celgene – Consultant, Grant/Research Support. Celltrion – Consultant. Exact Sciences – Stock-publicly held company(excluding mutual/index funds). Fresenius Kabi – Consultant. Genentech – Consultant, Grant/Research Support. Gilead – Consultant, Grant/Research Support. GlaxoSmithKline – Consultant. Gossamer Bio – Consultant, Grant/Research Support. Iota Biosciences – Consultant. Iterative Scopes – Consultant. Janssen – Consultant, Grant/Research Support. KSL Diagnostics – Consultant. Lilly – Consultant. Morphic – Consultant. Ono Pharma – Consultant. Pfizer – Consultant, Grant/Research Support. Protagonist – Consultant. Receptos – Grant/Research Support. Robarts Clinical Trials – Grant/Research Support. Scipher Medicine – Consultant. Sun Pharma – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support. Theravance – Grant/Research Support. UCB – Consultant, Grant/Research Support.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Gary Lichtenstein: AbbVie – Consultant. Allergan – CME. American College of Gastroenterology – Honorarium. American Gastroenterological Association – CME. American Regent (Creative Educational Concepts) – Consultant, Honorarium. Bristol Myers Squibb – Consultant, Grant/Research Support. Celgene – Consultant, Grant/Research Support. Chemed – CME. Eli Lilly – Advisor or Review Panel Member, Consultant. Endo Pharmaceuticals – Consultant. Ferring – Consultant. Focus Medical Communication – CME. Gastroenterology and Hepatology (Gastro-Hep Communications) – Honorarium. Gilead – Consultant. IBD Horizons – CME. IMEDEX – CME. Ironwood – CME. Janssen Orthobiotech – Consultant, Grant/Research Support, IBD Fellow Education Funding. Kabi Fresenius – Consultant. MedEd Consultants – Consultant. Merck – Consultant. Morphic Therapeutics – Consultant. Pennsylvania Society of Gastroenterology – CME. Pfizer Pharmaceuticals – Consultant, IBD Fellow Education Funding. Physician Education Resource – CME. Professional Communications, Inc. – Royalties. Prometheus Laboratories, Inc. – Consultant. Romark – Consultant, Honorarium. Salix Pharmaceuticals / Valeant – Consultant. Sandoz – Consultant. Shire Pharmaceuticals – Consultant. SLACK, Inc – Royalties. Springer Science and Business Media – Honorarium. Takeda – Consultant, Grant/Research Support. UCB – Consultant, Grant/Research Support. University of Kentucky – CME. Up-To-Date – Honorarium. Vindico – CME. Virgo – Consultant, Stock Options.
Aaron DuVall indicated no relevant financial relationships.
J. Casey Chapman: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Janssen – Speakers Bureau. Medtronic – Consultant. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Ana Lacerda: AbbVie – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Samuel Anyanwu: AbbVie – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Daniel O’Brien: AbbVie, Inc. – Employee.
Jianzhong Liu: AbbVie – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Andrew Garrison: AbbVie – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Marla Dubinsky: AbbVie – received consulting fees and/or acted as an advisor. Abivax – received consulting fees and/or acted as an advisor. AstraZeneca – received consulting fees and/or acted as an advisor. Bristol-Myers Squibb – received consulting fees and/or acted as an advisor. Eli Lilly – received consulting fees and/or acted as an advisor. Gilead – received consulting fees and/or acted as an advisor. Janssen – received consulting fees and/or acted as an advisor. Merck – received consulting fees and/or acted as an advisor. Pfizer – received consulting fees and/or acted as an advisor. Prometheus Biosciences – received consulting fees and/or acted as an advisor. Prometheus Labs – received consulting fees and/or acted as an advisor. Takeda – received consulting fees and/or acted as an advisor.
David T. Rubin, MD, FACG1, Edward V.. Loftus, MD2, Miguel Regueiro, MD3, Gary Lichtenstein, MD4, Aaron DuVall, MD5, J. Casey Chapman, MD6, Ana P.. Lacerda, MD, MSc7, Samuel I.. Anyanwu, PhD, MS7, Daniel O’Brien, PhD8, Jianzhong Liu, MD, MS7, Andrew Garrison, MS7, Marla C.. Dubinsky, MD9. P0732 - Efficacy of Upadacitinib in Patients With Crohn’s Disease Activity Index-Based Eligibility Criteria: Post Hoc Analysis of U-EXCEL, U-EXCEED, and U-ENDURE Phase 3 Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
