Sunday Poster Session
Category: IBD
P0753 - How Education Facilitated Uptake of a Novel Point of Care Decision Aid in IBD: The IBD Clinical Decision Support Tool
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Elizabeth Johnson, MA
RMEI
Voorhees, NJ
Presenting Author(s)
Elizabeth Johnson, MA1, Nicolette Theriault, MPH1, Margaret Stefan, MS1, Lobna Eldasher, PharmD1, Parambir S. Dulai, MD2
1RMEI, Voorhees, NJ; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
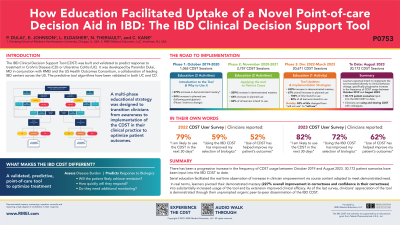
Introduction: Between launch in 2019 and the expiration of the most recent education program in January 2023, the IBD Clinical Decision Support Tool (CDST) was accessed a total of 24,493 times. 1,819 users have completed the curricula and 79 of those learners have responded to standalone follow-up surveys regarding their experience using the CDST in clinical practice. This multiphase educational program facilitated the utilization of a novel tool which will streamline the personalization of treatment. This strategy achieved real behavior change through the successive presentation of real-world case scenarios contextualized by experts discussing strategies to overcome challenges and barriers to implementation.
Methods: Non-randomized Pre and Post tests evaluated uptake of factual (Knowledge) and procedural (Competence) course content as well as self-reported confidence and intent to perform. The ratio of change between testing conditions was the metric by which increases in proficiency were determined. Changes in population proficiency were analyzed in the context of demographic and attitudinal data to qualify the targeting and content of future education. Additionally, a follow-up survey was distributed to learners who used the CDST subsequent to their participation in the education which investigated their experience implementing the tool in their clinical practice.
Results: Educational phases 1 & 2 (10/19 - 11/21) accrued 3,822 sessions. Phase 3 (12/21 -1/23) has 20,671 sessions to date. After participating in the most recent activity (Phase 3), 82% of GIs changed from “will not use the tool” to “will use the tool”, resulting in 100% of participating GIs intending to use the CDST. In a follow-up survey (N = 79), 67% of respondents reported that they agree or strongly agree that using the tool improved their decision making, and 61% observed that using the tool helped improve patient outcomes.
Discussion: Serial education facilitated the real time observation of increases in clinician empowerment via course content adapted to meet demonstrated need. In real terms, learners pivoted their demonstrated mastery (226% overall improvement in correctness and confidence in their correctness) into substantially increased usage of the tool and by extension improved clinical efficacy.
Disclosures:
Elizabeth Johnson, MA1, Nicolette Theriault, MPH1, Margaret Stefan, MS1, Lobna Eldasher, PharmD1, Parambir S. Dulai, MD2. P0753 - How Education Facilitated Uptake of a Novel Point of Care Decision Aid in IBD: The IBD Clinical Decision Support Tool, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1RMEI, Voorhees, NJ; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Between launch in 2019 and the expiration of the most recent education program in January 2023, the IBD Clinical Decision Support Tool (CDST) was accessed a total of 24,493 times. 1,819 users have completed the curricula and 79 of those learners have responded to standalone follow-up surveys regarding their experience using the CDST in clinical practice. This multiphase educational program facilitated the utilization of a novel tool which will streamline the personalization of treatment. This strategy achieved real behavior change through the successive presentation of real-world case scenarios contextualized by experts discussing strategies to overcome challenges and barriers to implementation.
Methods: Non-randomized Pre and Post tests evaluated uptake of factual (Knowledge) and procedural (Competence) course content as well as self-reported confidence and intent to perform. The ratio of change between testing conditions was the metric by which increases in proficiency were determined. Changes in population proficiency were analyzed in the context of demographic and attitudinal data to qualify the targeting and content of future education. Additionally, a follow-up survey was distributed to learners who used the CDST subsequent to their participation in the education which investigated their experience implementing the tool in their clinical practice.
Results: Educational phases 1 & 2 (10/19 - 11/21) accrued 3,822 sessions. Phase 3 (12/21 -1/23) has 20,671 sessions to date. After participating in the most recent activity (Phase 3), 82% of GIs changed from “will not use the tool” to “will use the tool”, resulting in 100% of participating GIs intending to use the CDST. In a follow-up survey (N = 79), 67% of respondents reported that they agree or strongly agree that using the tool improved their decision making, and 61% observed that using the tool helped improve patient outcomes.
Discussion: Serial education facilitated the real time observation of increases in clinician empowerment via course content adapted to meet demonstrated need. In real terms, learners pivoted their demonstrated mastery (226% overall improvement in correctness and confidence in their correctness) into substantially increased usage of the tool and by extension improved clinical efficacy.
Disclosures:
Elizabeth Johnson indicated no relevant financial relationships.
Nicolette Theriault indicated no relevant financial relationships.
Margaret Stefan indicated no relevant financial relationships.
Lobna Eldasher indicated no relevant financial relationships.
Parambir S. Dulai: Abbvie – Consultant. Abivax – Consultant. Adiso Therapeutics, Inc – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support. GlaxoSmithKline – Consultant. Janssen – Consultant, Grant/Research Support. Lilly – Consultant. Pfizer – Consultant, Grant/Research Support. PreciDiag – Royalties. Roivant – Consultant. Takeda – Consultant, Grant/Research Support.
Elizabeth Johnson, MA1, Nicolette Theriault, MPH1, Margaret Stefan, MS1, Lobna Eldasher, PharmD1, Parambir S. Dulai, MD2. P0753 - How Education Facilitated Uptake of a Novel Point of Care Decision Aid in IBD: The IBD Clinical Decision Support Tool, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
