Sunday Poster Session
Category: IBD
P0754 - In-Hospital Outcomes of Opioid-Dependent Inflammatory Bowel Disease in Cannabis vs Non-Cannabis Users: A Nationwide Propensity Matched Analysis in the United States
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- RK
Rewanth Katamreddy, MD
Saint Michael’s Medical Center
Newark, New Jersey
Presenting Author(s)
Rewanth Katamreddy, MD1, Samuel Edusa, MD2, Yamini Katamreddy, MD3, Ummul Asfeen, DO4, Jayasree Ravilla, MD5, Ali Tariq Alvi, MD6, Charu Agarwal, MBBS7, Birimroz Singh Sibia, MBBS8, Aleen Rahman, MBBS9, Fnu Vikash, MD10, Rupak Desai, MBBS11
1Saint Michael’s Medical Center, Newark, NJ; 2Piedmont Athens Regional, Athens, GA; 3West Anaheim Medical Center, Anaheim, CA; 4NYMC-Saint Michaels Medical Center, Newark, NJ; 5Monmouth Medical Center/RWJBH, Long Branch, NJ; 6HCA Florida Westside Hospital, Plantation, FL; 7Sri Sidhartha Medical College, Aurora, IL; 8KMC-Manipal, Manipal, Karnataka, India; 9Fatima Jinnah Medical University, San Jose, CA; 10Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 11Outcomes Research, Atlanta, GA
Introduction: According to the literature, Inflammatory Bowel Disease (IBD) patients with opioid dependency have a threefold higher mortality risk than non-users. Some studies suggest the role of cannabis usage in IBD due to its anti-inflammatory properties. However, no literature indicates the impact of cannabis usage on opioid-dependent IBD. Using a national propensity-matched sample, we assessed inpatient hospital outcomes of opioid-dependent IBD patients with Cannabis Use Disorder (CUD) versus non-CUD.
Methods: The Nationwide Inpatient Sample database (2019) was queried to identify opioid-dependent IBD in CUD versus non-CUD cohorts. A Pearson Chi-square test and Mann-Whitney U tests were used to compare categorical and continuous variables between propensity-matched cohorts. In-hospital complications were the primary outcome; Length-Of-Stay and hospital expenses were secondary.
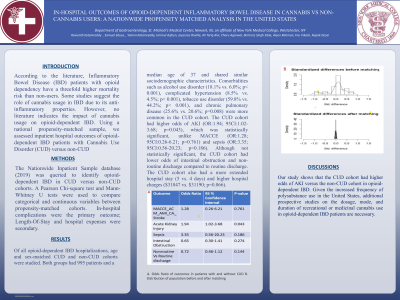
Results: Of all opioid-dependent IBD hospitalizations, age and sex-matched CUD and non-CUD cohorts were studied. Both groups had 995 patients and a median age of 37 and shared similar sociodemographic characteristics. Comorbidities such as alcohol use disorder (18.1% vs. 6.0%; p< 0.001), complicated hypertension (8.5% vs. 4.5%; p< 0.001), tobacco use disorder (59.8% vs. 44.2%; p< 0.001), and chronic pulmonary disease (25.6% vs. 20.6%; p=0.008) were more common in the CUD cohort. The CUD cohort had higher odds of AKI (OR:1.94; 95CI:1.02-3.68; p=0.043), which was statistically significant, unlike MACCE (OR:1.28; 95CI:0.26-6.21; p=0.761) and sepsis (OR:3.35; 95CI:0.56-20.23; p=0.186). Although not statistically significant, the CUD cohort had lower odds of intestinal obstruction and non-routine discharge compared to routine discharge. The CUD cohort also had a more extended hospital stay (5 vs. 4 days) and higher hospital charges ($31847 vs. $31190; p=0.066).
Discussion: Our study shows that the CUD cohort had higher odds of AKI versus the non-CUD cohort in opioid-dependent IBD. Given the increased frequency of polysubstance use in the United States, additional prospective studies on the dosage, mode, and duration of recreational or medicinal cannabis use in opioid-dependent IBD patients are necessary.

Disclosures:
Rewanth Katamreddy, MD1, Samuel Edusa, MD2, Yamini Katamreddy, MD3, Ummul Asfeen, DO4, Jayasree Ravilla, MD5, Ali Tariq Alvi, MD6, Charu Agarwal, MBBS7, Birimroz Singh Sibia, MBBS8, Aleen Rahman, MBBS9, Fnu Vikash, MD10, Rupak Desai, MBBS11. P0754 - In-Hospital Outcomes of Opioid-Dependent Inflammatory Bowel Disease in Cannabis vs Non-Cannabis Users: A Nationwide Propensity Matched Analysis in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Michael’s Medical Center, Newark, NJ; 2Piedmont Athens Regional, Athens, GA; 3West Anaheim Medical Center, Anaheim, CA; 4NYMC-Saint Michaels Medical Center, Newark, NJ; 5Monmouth Medical Center/RWJBH, Long Branch, NJ; 6HCA Florida Westside Hospital, Plantation, FL; 7Sri Sidhartha Medical College, Aurora, IL; 8KMC-Manipal, Manipal, Karnataka, India; 9Fatima Jinnah Medical University, San Jose, CA; 10Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 11Outcomes Research, Atlanta, GA
Introduction: According to the literature, Inflammatory Bowel Disease (IBD) patients with opioid dependency have a threefold higher mortality risk than non-users. Some studies suggest the role of cannabis usage in IBD due to its anti-inflammatory properties. However, no literature indicates the impact of cannabis usage on opioid-dependent IBD. Using a national propensity-matched sample, we assessed inpatient hospital outcomes of opioid-dependent IBD patients with Cannabis Use Disorder (CUD) versus non-CUD.
Methods: The Nationwide Inpatient Sample database (2019) was queried to identify opioid-dependent IBD in CUD versus non-CUD cohorts. A Pearson Chi-square test and Mann-Whitney U tests were used to compare categorical and continuous variables between propensity-matched cohorts. In-hospital complications were the primary outcome; Length-Of-Stay and hospital expenses were secondary.
Results: Of all opioid-dependent IBD hospitalizations, age and sex-matched CUD and non-CUD cohorts were studied. Both groups had 995 patients and a median age of 37 and shared similar sociodemographic characteristics. Comorbidities such as alcohol use disorder (18.1% vs. 6.0%; p< 0.001), complicated hypertension (8.5% vs. 4.5%; p< 0.001), tobacco use disorder (59.8% vs. 44.2%; p< 0.001), and chronic pulmonary disease (25.6% vs. 20.6%; p=0.008) were more common in the CUD cohort. The CUD cohort had higher odds of AKI (OR:1.94; 95CI:1.02-3.68; p=0.043), which was statistically significant, unlike MACCE (OR:1.28; 95CI:0.26-6.21; p=0.761) and sepsis (OR:3.35; 95CI:0.56-20.23; p=0.186). Although not statistically significant, the CUD cohort had lower odds of intestinal obstruction and non-routine discharge compared to routine discharge. The CUD cohort also had a more extended hospital stay (5 vs. 4 days) and higher hospital charges ($31847 vs. $31190; p=0.066).
Discussion: Our study shows that the CUD cohort had higher odds of AKI versus the non-CUD cohort in opioid-dependent IBD. Given the increased frequency of polysubstance use in the United States, additional prospective studies on the dosage, mode, and duration of recreational or medicinal cannabis use in opioid-dependent IBD patients are necessary.

Figure: A. Odds Ratio of outcomes in patients with and without CUD
B. Distribution of population before and after matching
B. Distribution of population before and after matching
Disclosures:
Rewanth Katamreddy indicated no relevant financial relationships.
Samuel Edusa indicated no relevant financial relationships.
Yamini Katamreddy indicated no relevant financial relationships.
Ummul Asfeen indicated no relevant financial relationships.
Jayasree Ravilla indicated no relevant financial relationships.
Ali Tariq Alvi indicated no relevant financial relationships.
Charu Agarwal indicated no relevant financial relationships.
Birimroz Singh Sibia indicated no relevant financial relationships.
Aleen Rahman indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Rewanth Katamreddy, MD1, Samuel Edusa, MD2, Yamini Katamreddy, MD3, Ummul Asfeen, DO4, Jayasree Ravilla, MD5, Ali Tariq Alvi, MD6, Charu Agarwal, MBBS7, Birimroz Singh Sibia, MBBS8, Aleen Rahman, MBBS9, Fnu Vikash, MD10, Rupak Desai, MBBS11. P0754 - In-Hospital Outcomes of Opioid-Dependent Inflammatory Bowel Disease in Cannabis vs Non-Cannabis Users: A Nationwide Propensity Matched Analysis in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
