Sunday Poster Session
Category: IBD
P0758 - Are Psychosocial Risk Factors Associated With Increased Readmissions in Inflammatory Bowel Disease in the COVID-19 Era?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Aakriti Soni, MD
Saint Vincent Hospital
Worcester, MA
Presenting Author(s)
Aakriti Soni, MD, Kannu Bansal, MD, Anuroop Yekula, MD, Mithil Gowda Suresh, MD, Suchet Singh Randhawa, MD, George M. Abraham, MD
Saint Vincent Hospital, Worcester, MA
Introduction: Psychosocial risk factors (PSRFs) have gained recognition as important non-traditional factors that influence outcomes in patients with Inflammatory Bowel Disease (IBD). However, there is a lack of sufficient data on the study of these risk factors in IBD at a national level. Furthermore, the impact of these factors during the challenging times of COVID-19 pandemic remains unexplored.
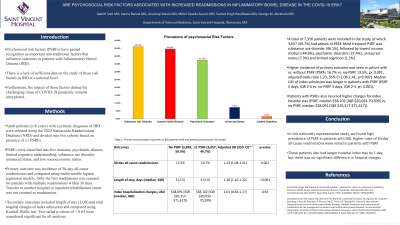
Methods: Adult patients (≥18 years) with a primary diagnosis of IBD were selected using the 2020 Nationwide Readmissions Database (NRD) and divided into two cohorts based on presence of ≥1 PSRFs. PSRFs were classified into five domains: psychiatric disease, limited cognitive understanding, substance use disorder, uninsured status, and low socioeconomic status.
Primary outcome was incidence of 30-day all-cause readmissions and compared using multivariable logistic regression models. Only the first readmission was counted for patients with multiple readmissions within 30 days. Transfer to another hospital or inpatient rehabilitation center was not counted as readmission. Secondary outcomes included length of stay (LOS) and total hospital charges of index admission and compared using Kruskal-Wallis test. Two-tailed p-values of < 0.05 were considered significant for all analyses.
Results: A total of 7,356 patients were included in the study, of which 3,657 (49.7%) had atleast ≥1PSRF. Most frequent PSRF was substance use disorder (46.1%), followed by lowest income stratum (44.6%), psychiatric disorders (37.4%), uninsured status (7.3%) and limited cognition (1.5%). Higher incidence of primary outcome was seen in cohort with vs. without PSRF (PSRFs 16.7% vs. no-PSRF 13.5%, p< 0.001; adjusted odds ratio 1.23, 95% CI 1.08-1.41, p=0.002). Median LOS of index admission was longer in patients with PSRF (PSRF 4 days, IQR 2-6 vs. no-PSRF 3 days, IQR 2-5, p< 0.001). Patients with PSRFs also incurred higher charges for index hospital stay (PSRF, median $38,102 [IQR $20,033-70,309] vs. no PSRF, median $38,091 [IQR $20,317-$71,617]).
Discussion: In this nationally representative study, we found high prevalence of PSRF in patients with IBD. Higher rates of 30-day all-cause readmissions were noted in patients with PSRF. These patients also had longer hospital index stay by 1 day, but there was no significant difference in hospital charges.
Disclosures:
Aakriti Soni, MD, Kannu Bansal, MD, Anuroop Yekula, MD, Mithil Gowda Suresh, MD, Suchet Singh Randhawa, MD, George M. Abraham, MD. P0758 - Are Psychosocial Risk Factors Associated With Increased Readmissions in Inflammatory Bowel Disease in the COVID-19 Era?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Saint Vincent Hospital, Worcester, MA
Introduction: Psychosocial risk factors (PSRFs) have gained recognition as important non-traditional factors that influence outcomes in patients with Inflammatory Bowel Disease (IBD). However, there is a lack of sufficient data on the study of these risk factors in IBD at a national level. Furthermore, the impact of these factors during the challenging times of COVID-19 pandemic remains unexplored.
Methods: Adult patients (≥18 years) with a primary diagnosis of IBD were selected using the 2020 Nationwide Readmissions Database (NRD) and divided into two cohorts based on presence of ≥1 PSRFs. PSRFs were classified into five domains: psychiatric disease, limited cognitive understanding, substance use disorder, uninsured status, and low socioeconomic status.
Primary outcome was incidence of 30-day all-cause readmissions and compared using multivariable logistic regression models. Only the first readmission was counted for patients with multiple readmissions within 30 days. Transfer to another hospital or inpatient rehabilitation center was not counted as readmission. Secondary outcomes included length of stay (LOS) and total hospital charges of index admission and compared using Kruskal-Wallis test. Two-tailed p-values of < 0.05 were considered significant for all analyses.
Results: A total of 7,356 patients were included in the study, of which 3,657 (49.7%) had atleast ≥1PSRF. Most frequent PSRF was substance use disorder (46.1%), followed by lowest income stratum (44.6%), psychiatric disorders (37.4%), uninsured status (7.3%) and limited cognition (1.5%). Higher incidence of primary outcome was seen in cohort with vs. without PSRF (PSRFs 16.7% vs. no-PSRF 13.5%, p< 0.001; adjusted odds ratio 1.23, 95% CI 1.08-1.41, p=0.002). Median LOS of index admission was longer in patients with PSRF (PSRF 4 days, IQR 2-6 vs. no-PSRF 3 days, IQR 2-5, p< 0.001). Patients with PSRFs also incurred higher charges for index hospital stay (PSRF, median $38,102 [IQR $20,033-70,309] vs. no PSRF, median $38,091 [IQR $20,317-$71,617]).
Discussion: In this nationally representative study, we found high prevalence of PSRF in patients with IBD. Higher rates of 30-day all-cause readmissions were noted in patients with PSRF. These patients also had longer hospital index stay by 1 day, but there was no significant difference in hospital charges.
Disclosures:
Aakriti Soni indicated no relevant financial relationships.
Kannu Bansal indicated no relevant financial relationships.
Anuroop Yekula indicated no relevant financial relationships.
Mithil Gowda Suresh indicated no relevant financial relationships.
Suchet Singh Randhawa indicated no relevant financial relationships.
George M. Abraham indicated no relevant financial relationships.
Aakriti Soni, MD, Kannu Bansal, MD, Anuroop Yekula, MD, Mithil Gowda Suresh, MD, Suchet Singh Randhawa, MD, George M. Abraham, MD. P0758 - Are Psychosocial Risk Factors Associated With Increased Readmissions in Inflammatory Bowel Disease in the COVID-19 Era?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
