Sunday Poster Session
Category: IBD
P0784 - The Impact of Early vs Late COVID-19 on IBD-Related Disease Activity, Course, and Exacerbations
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Khaled Alsabbagh Alchirazi, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Alia Khamis, MD2, Aakash Desai, MD3, Thabet Qapaja, MD1, Osama Hamid, MD, MRCPI1, Nour Azzouz, MD1, Miguel Regueiro, MD4
1Cleveland Clinic, Cleveland, OH; 2University of Rochester Medical Center, Rochester, NY; 3MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 4Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: The COVID-19 pandemic, caused by novel coronavirus SARS-CoV-2, created ambiguity in managing IBD due to insufficient data of the relationship between both diseases. This resulted in multiple studies aiming to assess patterns that could be impactful in managing those patients who are affected. Most of these studies focused on the risk and severity of COVID infections in inflammatory bowel disease (IBD) patients. We aim to evaluate the impact of COVID infection on IBD-related disease activity in early vs late pandemic.
Methods: We conducted a retrospective cohort study using TriNetX, a multi-institutional database to assess the impact of COVID infection on patients with IBD compared with IBD patients without COVID-19 infection in early (3/1/2020 and 3/1/2021) vs late (3/2/2021 and 3/2/2022) periods of the pandemic, both groups were followed up to 1 year of COVID-19 infection. 1:1 propensity score matching was performed for Age, Gender, Race, IBD medications, autoimmune diseases, IBD subtype and phenotype and prior IBD related surgery. Risk was expressed as adjusted odds ratio (aOR) with 95% confidence intervals (CI).
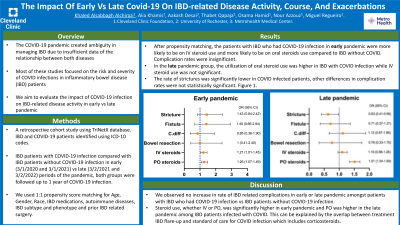
Results: After propensity score matching, the patients with IBD who had COVID-19 infection in early pandemic were more likely to be on IV steroid use and more likely to be on oral steroids use compared to IBD without COVID. Complication rates including small bowel or colon surgery, Clostridium difficile infection, and development of strictures or fistula among both groups were insignificant. In the late pandemic group, the utilization of oral steroid use was significantly higher in IBD with COVID infection while IV steroid use was not significant. The rate of strictures was significantly lower in COVID infected patients, other differences in complication rates were not statistically significant. Figure 1.
Discussion: We observed no increase in rate of IBD related complications in early or late pandemic amongst patients with IBD who had COVID-19 infection vs IBD patients without COVID-19 infection. Some of the complications do take years to develop and thus a longer follow-up time is required to measure a difference. Steroid use, whether IV or PO, was significantly higher in early pandemic and PO was higher in the late pandemic among IBD patients infected with COVID. This can be explained by the overlap between treatment IBD flare-up and standard of care for COVID infection which includes corticosteroids.

Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Alia Khamis, MD2, Aakash Desai, MD3, Thabet Qapaja, MD1, Osama Hamid, MD, MRCPI1, Nour Azzouz, MD1, Miguel Regueiro, MD4. P0784 - The Impact of Early vs Late COVID-19 on IBD-Related Disease Activity, Course, and Exacerbations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Rochester Medical Center, Rochester, NY; 3MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH; 4Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH
Introduction: The COVID-19 pandemic, caused by novel coronavirus SARS-CoV-2, created ambiguity in managing IBD due to insufficient data of the relationship between both diseases. This resulted in multiple studies aiming to assess patterns that could be impactful in managing those patients who are affected. Most of these studies focused on the risk and severity of COVID infections in inflammatory bowel disease (IBD) patients. We aim to evaluate the impact of COVID infection on IBD-related disease activity in early vs late pandemic.
Methods: We conducted a retrospective cohort study using TriNetX, a multi-institutional database to assess the impact of COVID infection on patients with IBD compared with IBD patients without COVID-19 infection in early (3/1/2020 and 3/1/2021) vs late (3/2/2021 and 3/2/2022) periods of the pandemic, both groups were followed up to 1 year of COVID-19 infection. 1:1 propensity score matching was performed for Age, Gender, Race, IBD medications, autoimmune diseases, IBD subtype and phenotype and prior IBD related surgery. Risk was expressed as adjusted odds ratio (aOR) with 95% confidence intervals (CI).
Results: After propensity score matching, the patients with IBD who had COVID-19 infection in early pandemic were more likely to be on IV steroid use and more likely to be on oral steroids use compared to IBD without COVID. Complication rates including small bowel or colon surgery, Clostridium difficile infection, and development of strictures or fistula among both groups were insignificant. In the late pandemic group, the utilization of oral steroid use was significantly higher in IBD with COVID infection while IV steroid use was not significant. The rate of strictures was significantly lower in COVID infected patients, other differences in complication rates were not statistically significant. Figure 1.
Discussion: We observed no increase in rate of IBD related complications in early or late pandemic amongst patients with IBD who had COVID-19 infection vs IBD patients without COVID-19 infection. Some of the complications do take years to develop and thus a longer follow-up time is required to measure a difference. Steroid use, whether IV or PO, was significantly higher in early pandemic and PO was higher in the late pandemic among IBD patients infected with COVID. This can be explained by the overlap between treatment IBD flare-up and standard of care for COVID infection which includes corticosteroids.

Figure: Figure 1: Impact of COVID-19 on patients with IBD in early (A) vs late pandemic (B) compared with IBD patients without COVID infection after propensity score matching.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Alia Khamis indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Thabet Qapaja indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Nour Azzouz indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Khaled Alsabbagh Alchirazi, MD1, Alia Khamis, MD2, Aakash Desai, MD3, Thabet Qapaja, MD1, Osama Hamid, MD, MRCPI1, Nour Azzouz, MD1, Miguel Regueiro, MD4. P0784 - The Impact of Early vs Late COVID-19 on IBD-Related Disease Activity, Course, and Exacerbations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
