Sunday Poster Session
Category: IBD
P0786 - Racial Disparities in Venous Thromboembolism Subtypes in IBD: A Five-Year Population-Based Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- YK
Yassine Kilani, MD
Lincoln Medical Center
New York, NY
Presenting Author(s)
Yassine Kilani, MD1, Syeda Ashna Fatima Kamal, MD2, Mohammad Aldiabat, MD3, Saqr Alsakarneh, MD4, Iqra Arshad, MD1, Priscila Castro Puello, MD1, Fnu Vikash, MD5, Vikash Kumar, MD6
1Lincoln Medical Center, New York, NY; 2SIU School of Medicine, Springfield, IL; 3NYU Langone, New York, NY; 4University of Missouri-Kansas City, Kansas City, MO; 5Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 6Brooklyn Hospital Center, Brooklyn, NY
Introduction: Inflammatory bowel disease (IBD) has been associated with an increased risk of venous thromboembolism (VTE). However, there is currently no literature describing racial disparities among thrombotic manifestations of IBD. Therefore, authors of this study aimed to identify potential disparities in the prevalence and risks of VTE among different races of individuals with IBD.
Methods: This is a retrospective longitudinal study of patients with IBD, admitted with a primary diagnosis of VTE, including deep vein thrombosis (DVT) and pulmonary embolism (PE). Using weighted data from the Nationwide Inpatient Sample (NIS) database from 2016 to 2020, we assessed outcomes (mortality, hospital utilization, total healthcare charges, complications) of patients admitted with VTE in the context of IBD. Baseline characteristics were analyzed using T-test and Chi-Square, and a multivariate regression analysis was used to estimate outcomes between races. Data analysis was performed using STATA® Version 17.0/SE Software, with statistical significance set at p < 0.05.
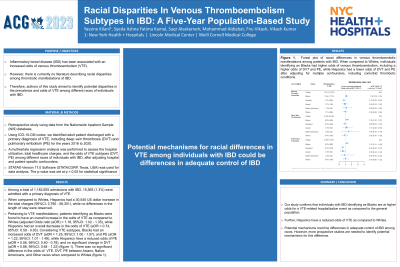
Results: Among a total of 1,182,655 admissions with IBD, 15,565 (1.3%) were admitted with a primary diagnosis of VTE. When compared to Whites, Hispanics had a 30,545 US dollar increase in the total charges (95%CI: 2,790 - 58,301), while no differences in the length of stay were observed. Pertaining to VTE manifestations, patients identifying as Blacks were found to have an overall increase in the risk of VTE as compared to Whites (adjusted Odds ratio (aOR) = 1.18, 95%CI: 1.02 - 1.35), while Hispanics had an overall decrease in the VTE risk (aOR = 0.74, 95%CI: 0.59 - 0.93). Considering VTE subtypes, Blacks had an increased risk of DVT (aOR = 1.25, 95%CI: 1.00 - 1.57), and PE (aOR = 1.22, 95%CI: 1.01 - 1.48), while Hispanics have a reduced risk of PE (aOR = 0.56, 95%CI: 0.40 - 0.78), and no significant change in DVT (aOR = 0.88, 95%CI: 0.64 - 1.22) (figure 1). There was no significant difference in the risk of VTE, DVT, PE between Asians, Native Americans, and Other races when compared to Whites (figure 1).
Discussion: Our study confirms that individuals with IBD identifying as Blacks are at higher risk for a VTE-related hospitalization event as compared to the general population. Further, Hispanics have a reduced risk of VTE as compared to Whites. Potential mechanisms could be differences in adequate control of IBD among races. However, more prospective studies are needed to identify potential mechanisms for this difference.

Disclosures:
Yassine Kilani, MD1, Syeda Ashna Fatima Kamal, MD2, Mohammad Aldiabat, MD3, Saqr Alsakarneh, MD4, Iqra Arshad, MD1, Priscila Castro Puello, MD1, Fnu Vikash, MD5, Vikash Kumar, MD6. P0786 - Racial Disparities in Venous Thromboembolism Subtypes in IBD: A Five-Year Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lincoln Medical Center, New York, NY; 2SIU School of Medicine, Springfield, IL; 3NYU Langone, New York, NY; 4University of Missouri-Kansas City, Kansas City, MO; 5Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 6Brooklyn Hospital Center, Brooklyn, NY
Introduction: Inflammatory bowel disease (IBD) has been associated with an increased risk of venous thromboembolism (VTE). However, there is currently no literature describing racial disparities among thrombotic manifestations of IBD. Therefore, authors of this study aimed to identify potential disparities in the prevalence and risks of VTE among different races of individuals with IBD.
Methods: This is a retrospective longitudinal study of patients with IBD, admitted with a primary diagnosis of VTE, including deep vein thrombosis (DVT) and pulmonary embolism (PE). Using weighted data from the Nationwide Inpatient Sample (NIS) database from 2016 to 2020, we assessed outcomes (mortality, hospital utilization, total healthcare charges, complications) of patients admitted with VTE in the context of IBD. Baseline characteristics were analyzed using T-test and Chi-Square, and a multivariate regression analysis was used to estimate outcomes between races. Data analysis was performed using STATA® Version 17.0/SE Software, with statistical significance set at p < 0.05.
Results: Among a total of 1,182,655 admissions with IBD, 15,565 (1.3%) were admitted with a primary diagnosis of VTE. When compared to Whites, Hispanics had a 30,545 US dollar increase in the total charges (95%CI: 2,790 - 58,301), while no differences in the length of stay were observed. Pertaining to VTE manifestations, patients identifying as Blacks were found to have an overall increase in the risk of VTE as compared to Whites (adjusted Odds ratio (aOR) = 1.18, 95%CI: 1.02 - 1.35), while Hispanics had an overall decrease in the VTE risk (aOR = 0.74, 95%CI: 0.59 - 0.93). Considering VTE subtypes, Blacks had an increased risk of DVT (aOR = 1.25, 95%CI: 1.00 - 1.57), and PE (aOR = 1.22, 95%CI: 1.01 - 1.48), while Hispanics have a reduced risk of PE (aOR = 0.56, 95%CI: 0.40 - 0.78), and no significant change in DVT (aOR = 0.88, 95%CI: 0.64 - 1.22) (figure 1). There was no significant difference in the risk of VTE, DVT, PE between Asians, Native Americans, and Other races when compared to Whites (figure 1).
Discussion: Our study confirms that individuals with IBD identifying as Blacks are at higher risk for a VTE-related hospitalization event as compared to the general population. Further, Hispanics have a reduced risk of VTE as compared to Whites. Potential mechanisms could be differences in adequate control of IBD among races. However, more prospective studies are needed to identify potential mechanisms for this difference.

Figure: Figure 1. Forest plot of racial differences in venous thromboembolic manifestations among patients with IBD. When compared to Whites, individuals identifying as Blacks had higher risks of venous thromboembolism, including a higher risk of DVT and PE, while Hispanics had a lower risks of DVT and PE after adjusting for multiple confounders, including comorbid thrombotic conditions.
Disclosures:
Yassine Kilani indicated no relevant financial relationships.
Syeda Ashna Fatima Kamal indicated no relevant financial relationships.
Mohammad Aldiabat indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Iqra Arshad indicated no relevant financial relationships.
Priscila Castro Puello indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Yassine Kilani, MD1, Syeda Ashna Fatima Kamal, MD2, Mohammad Aldiabat, MD3, Saqr Alsakarneh, MD4, Iqra Arshad, MD1, Priscila Castro Puello, MD1, Fnu Vikash, MD5, Vikash Kumar, MD6. P0786 - Racial Disparities in Venous Thromboembolism Subtypes in IBD: A Five-Year Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
