Sunday Poster Session
Category: IBD
P0805 - Olmesartan-Induced Enteropathy Mimicking Ileal and Duodenal Crohn’s Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Anastasia Naritsin, DO
Lahey Hospital and Medical Center
Woburn, MA
Presenting Author(s)
Anastasia Naritsin, DO1, Randall Pellish, MD2
1Lahey Hospital and Medical Center, Burlington, MA; 2Lahey Hospital, Burlington, MA
Introduction: Olmesartan, an angiotensin-receptor blocker used to treat hypertension became commercially available in 2002. Since 2012, it has been reported in cohorts as causing proximal small bowel inflammation that can mimic signs of celiac disease, including severe diarrhea, weight loss, and intestinal inflammation with villous atrophy on histopathology. The cohorts of olmesartan-induced celiac-like pathology have demonstrated proximal small intestinal inflammation which resolves with discontinuation of olmesartan. A more extensive, multifocal small bowel inflammatory process including luminal stricturing that mimics Crohn’s disease has not been reported.
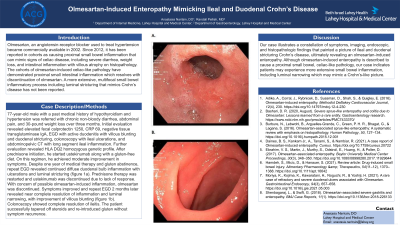
Case Description/Methods: 77-year-old male with a past medical history of hypothyroidism and hypertension was referred with chronic non-bloody diarrhea, abdominal pain, and 30-pound weight loss over three months. Initial evaluation revealed elevated fecal calprotectin 1250, CRP 69, negative tissue transglutaminase IgA, EGD with active duodenitis with villous blunting and duodenal stricturing, colonoscopy with ileal ulcerations, and abdominopelvic CT with long segment ileal inflammation. Further evaluation revealed HLA DQ2 homozygous genetic profile. After prednisone initiation, he started ustekinumab along with a gluten-free diet. On this regimen, he achieved moderate improvement in symptoms. Despite one year of medical therapy and gluten abstinence, repeat EGD revealed continued diffuse duodenal bulb inflammation with ulcerations and luminal stricturing (figure 1a). Prednisone therapy was restarted and ustekinumab was discontinued due to lack of response. With concern of possible olmesartan-induced inflammation, olmesartan was discontinued. Symptoms improved and repeat EGD 2 months later revealed near complete resolution of inflammation and luminal narrowing, with improvement of villous blunting (figure 1b). Colonoscopy showed complete resolution of ileitis. The patient successfully tapered off steroids and re-introduced gluten without symptom recurrence.
Discussion: Our case illustrates a constellation of symptoms, imaging, endoscopic, and histopathologic findings that painted a picture of ileal and duodenal stricturing Crohn’s disease, ultimately revealing an olmesartan-induced enteropathy. Although olmesartan-induced enteropathy is described to cause a proximal small bowel, celiac-like pathology, our case indicates patients may experience more extensive small bowel inflammation, including luminal narrowing which may mimic a Crohn’s-like picture.

Disclosures:
Anastasia Naritsin, DO1, Randall Pellish, MD2. P0805 - Olmesartan-Induced Enteropathy Mimicking Ileal and Duodenal Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lahey Hospital and Medical Center, Burlington, MA; 2Lahey Hospital, Burlington, MA
Introduction: Olmesartan, an angiotensin-receptor blocker used to treat hypertension became commercially available in 2002. Since 2012, it has been reported in cohorts as causing proximal small bowel inflammation that can mimic signs of celiac disease, including severe diarrhea, weight loss, and intestinal inflammation with villous atrophy on histopathology. The cohorts of olmesartan-induced celiac-like pathology have demonstrated proximal small intestinal inflammation which resolves with discontinuation of olmesartan. A more extensive, multifocal small bowel inflammatory process including luminal stricturing that mimics Crohn’s disease has not been reported.
Case Description/Methods: 77-year-old male with a past medical history of hypothyroidism and hypertension was referred with chronic non-bloody diarrhea, abdominal pain, and 30-pound weight loss over three months. Initial evaluation revealed elevated fecal calprotectin 1250, CRP 69, negative tissue transglutaminase IgA, EGD with active duodenitis with villous blunting and duodenal stricturing, colonoscopy with ileal ulcerations, and abdominopelvic CT with long segment ileal inflammation. Further evaluation revealed HLA DQ2 homozygous genetic profile. After prednisone initiation, he started ustekinumab along with a gluten-free diet. On this regimen, he achieved moderate improvement in symptoms. Despite one year of medical therapy and gluten abstinence, repeat EGD revealed continued diffuse duodenal bulb inflammation with ulcerations and luminal stricturing (figure 1a). Prednisone therapy was restarted and ustekinumab was discontinued due to lack of response. With concern of possible olmesartan-induced inflammation, olmesartan was discontinued. Symptoms improved and repeat EGD 2 months later revealed near complete resolution of inflammation and luminal narrowing, with improvement of villous blunting (figure 1b). Colonoscopy showed complete resolution of ileitis. The patient successfully tapered off steroids and re-introduced gluten without symptom recurrence.
Discussion: Our case illustrates a constellation of symptoms, imaging, endoscopic, and histopathologic findings that painted a picture of ileal and duodenal stricturing Crohn’s disease, ultimately revealing an olmesartan-induced enteropathy. Although olmesartan-induced enteropathy is described to cause a proximal small bowel, celiac-like pathology, our case indicates patients may experience more extensive small bowel inflammation, including luminal narrowing which may mimic a Crohn’s-like picture.

Figure: Title: Crohn's-Like Picture in Olmesartan-Induced Enteropathy
EGD showing resolution of duodenal stricturing after olmesartan discontinuation.
A: Duodenal stricturing on olmasartan
B: Resolution of duodenal striucturing off olmasartan
EGD showing resolution of duodenal stricturing after olmesartan discontinuation.
A: Duodenal stricturing on olmasartan
B: Resolution of duodenal striucturing off olmasartan
Disclosures:
Anastasia Naritsin indicated no relevant financial relationships.
Randall Pellish indicated no relevant financial relationships.
Anastasia Naritsin, DO1, Randall Pellish, MD2. P0805 - Olmesartan-Induced Enteropathy Mimicking Ileal and Duodenal Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
