Sunday Poster Session
Category: IBD
P0809 - An Atypical Malignancy in a Patient With IBD
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jellyana Peraza, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Jellyana Peraza, MD, Nicholas Scalzo, MD, Bhavana Bhagya Rao, MD
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Patients with inflammatory bowel disease (IBD) are known to be at increased risk of colorectal cancer (CRC). However, association with less common gastrointestinal (GI) malignancies is not well established
Case Description/Methods: A 74-year-old woman presented with chronic bloody diarrhea, nocturnal awakenings, and unintentional weight loss over the preceding six months. Colonoscopy for CRC screening done 3 years prior had been unremarkable. Her physical exam was most notable for pallor. Laboratory data revealed iron deficiency anemia (hemoglobin 6.4 g/dl), high C-reactive protein (46 mg/L), and elevated fecal calprotectin (6640 mcg/g). Computed tomography scan showed active on chronic proctocolitis and 2.7cm semi-annular asymmetric wall thickening in the distal transverse colon (TC) concerning for malignancy. Colonoscopy revealed Mayo 3 pancolitis consistent with severe ulcerative colitis (UC). In addition, a 3 cm fungating, polypoid mass was seen in the distal TC. Biopsies from the mass showed moderately active chronic colitis negative for dysplasia. Given the severity of colitis and concerns for false negative biopsies for CRC, patient underwent total colectomy and end ileostomy. Surgical pathology showed severely active chronic idiopathic ulcerative pancolitis and a 3-cm gastrointestinal stromal tumor (GIST), mostly spindle cell type, invading into the deep muscularis propria, with a mitotic index 3/5mm2 and with expression of CD117 and DOG1
Discussion: Patients with IBD are known to be at increased risk of GI cancer, likely due to chronic inflammation and exposure to immunomodulatory agents. CRC is encountered most often, with an annual incidence estimated at 76/100,000 py for UC. GISTs account for < 1% of all GI cancers across all patients. The incidence of GIST in IBD is unknown, and there is no evidence supporting an association between these two entities. The most common location of GISTs is the stomach (60%), and only 5% of GISTs are found in the colon. Diagnosis of GIST is challenging on endoscopy since it does not rise in the mucosal layer and is thus not amenable to sampling by standard biopsy techniques. Endoscopic ultrasound with fine needle biopsy is the modality of choice to evaluate GIST, but this is technically challenging for colonic lesions.
While IBD patients are known to be at increased risk of CRC, there is no evidence supporting the association between GIST and IBD. Endoscopic ultrasound-guided fine needle biopsy or surgical sampling is often needed to diagnose GIST

Disclosures:
Jellyana Peraza, MD, Nicholas Scalzo, MD, Bhavana Bhagya Rao, MD. P0809 - An Atypical Malignancy in a Patient With IBD, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Patients with inflammatory bowel disease (IBD) are known to be at increased risk of colorectal cancer (CRC). However, association with less common gastrointestinal (GI) malignancies is not well established
Case Description/Methods: A 74-year-old woman presented with chronic bloody diarrhea, nocturnal awakenings, and unintentional weight loss over the preceding six months. Colonoscopy for CRC screening done 3 years prior had been unremarkable. Her physical exam was most notable for pallor. Laboratory data revealed iron deficiency anemia (hemoglobin 6.4 g/dl), high C-reactive protein (46 mg/L), and elevated fecal calprotectin (6640 mcg/g). Computed tomography scan showed active on chronic proctocolitis and 2.7cm semi-annular asymmetric wall thickening in the distal transverse colon (TC) concerning for malignancy. Colonoscopy revealed Mayo 3 pancolitis consistent with severe ulcerative colitis (UC). In addition, a 3 cm fungating, polypoid mass was seen in the distal TC. Biopsies from the mass showed moderately active chronic colitis negative for dysplasia. Given the severity of colitis and concerns for false negative biopsies for CRC, patient underwent total colectomy and end ileostomy. Surgical pathology showed severely active chronic idiopathic ulcerative pancolitis and a 3-cm gastrointestinal stromal tumor (GIST), mostly spindle cell type, invading into the deep muscularis propria, with a mitotic index 3/5mm2 and with expression of CD117 and DOG1
Discussion: Patients with IBD are known to be at increased risk of GI cancer, likely due to chronic inflammation and exposure to immunomodulatory agents. CRC is encountered most often, with an annual incidence estimated at 76/100,000 py for UC. GISTs account for < 1% of all GI cancers across all patients. The incidence of GIST in IBD is unknown, and there is no evidence supporting an association between these two entities. The most common location of GISTs is the stomach (60%), and only 5% of GISTs are found in the colon. Diagnosis of GIST is challenging on endoscopy since it does not rise in the mucosal layer and is thus not amenable to sampling by standard biopsy techniques. Endoscopic ultrasound with fine needle biopsy is the modality of choice to evaluate GIST, but this is technically challenging for colonic lesions.
While IBD patients are known to be at increased risk of CRC, there is no evidence supporting the association between GIST and IBD. Endoscopic ultrasound-guided fine needle biopsy or surgical sampling is often needed to diagnose GIST

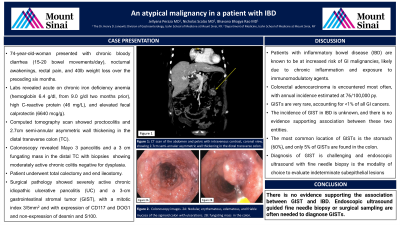
Figure: Figure 1: Computed tomography scan of the abdomen and pelvis with intravenous contrast, coronal view, showing 2.7cm semi-annular asymmetric wall thickening in the distal transverse colon.
Figure 2: Colonoscopy images. 2A: Nodular, erythematous, edematous, and friable mucosa of the sigmoid colon with ulcerations consistent with severe active UC. 2B: fungating, polypoid non-obstructing 3cm mass seen in the distal transverse colon and mucosal biopsies taken with biopsy forceps.
Figure 2: Colonoscopy images. 2A: Nodular, erythematous, edematous, and friable mucosa of the sigmoid colon with ulcerations consistent with severe active UC. 2B: fungating, polypoid non-obstructing 3cm mass seen in the distal transverse colon and mucosal biopsies taken with biopsy forceps.
Disclosures:
Jellyana Peraza indicated no relevant financial relationships.
Nicholas Scalzo indicated no relevant financial relationships.
Bhavana Bhagya Rao indicated no relevant financial relationships.
Jellyana Peraza, MD, Nicholas Scalzo, MD, Bhavana Bhagya Rao, MD. P0809 - An Atypical Malignancy in a Patient With IBD, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
