Sunday Poster Session
Category: IBD
P0810 - Peripheral Arterial Thrombosis: A Potential Complication in Inflammatory Bowel Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AK
Andrew Kim, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Andrew Kim, MD, Clemence C. White, DO, Roy Wong, MD, Katherine M. Whitehouse, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: As compared to venous thrombosis, arterial thrombosis is a very rare but well-recognized vascular complication of inflammatory bowel disease (IBD). The risk of thromboembolic events (TE) is proportionally associated to the severity of inflammation, particularly in hospitalized IBD patients. However, the pathogenesis of TE in IBD is not well understood. Current genetic studies have not demonstrated a specific etiology, suggesting a more prominent role for acquired factors. Understanding the risks that predispose IBD patients to arterial TE may further elucidate the pathogenesis of thrombosis and potential treatment points. We report a case of a 60yo F with extensive colitis and peripheral arterial thrombosis.
Case Description/Methods: 60-year-old obese female with extensive colitis, previously in remission for over ten years, presented to the emergency department with five day onset of abdominal pain, increased frequency of bowel movements, urgency, nocturnal events, and hematochezia. Her vital signs were within normal limits. Physical exam was notable for diffuse abdominal pain on palpation. Her laboratory studies revealed elevated inflammatory markers: Fecal calprotectin 2092 mcg/g, C-reactive protein 30.65 mg/dL, and white cell count 20.5 x 103/mcL. Stool culture and C. difficile PCR were negative. Abdominal Computed Tomography (CT) showed diffuse pan-colonic wall thickening. No discernible mass noted. She was started on intravenous steroids.
On hospital day 3, she complained of severe right leg pain. Physical exam revealed a mottled, pallorous limb with an absent tibial arterial pulse, concerning for acute limb ischemia. Patient was started on heparin anticoagulation and was evaluated by the vascular surgery team. Emergent angiogram confirmed the diagnosis. She underwent right femoral, popliteal, and tibial arterial thrombectomies. A hypercoagulable work-up by the hematology team was negative. Flexible sigmoidoscopy revealed diffuse large ulcers with biopsies negative for cytomegalovirus. The patient was transitioned to apixaban anticoagulation and oral prednisone taper. Infliximab was started.
Discussion: Peripheral arterial thrombosis is a rare complication in IBD with a reported incidence of less than 1 in 1000. Its pathogenesis is unknown. Our patient risk factors include obesity, gender, disease flare, and hospitalization. This case highlights the presence of arterial thrombosis in IBD and the need for continued case reporting, paramount to guide further investigations.

Disclosures:
Andrew Kim, MD, Clemence C. White, DO, Roy Wong, MD, Katherine M. Whitehouse, MD. P0810 - Peripheral Arterial Thrombosis: A Potential Complication in Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: As compared to venous thrombosis, arterial thrombosis is a very rare but well-recognized vascular complication of inflammatory bowel disease (IBD). The risk of thromboembolic events (TE) is proportionally associated to the severity of inflammation, particularly in hospitalized IBD patients. However, the pathogenesis of TE in IBD is not well understood. Current genetic studies have not demonstrated a specific etiology, suggesting a more prominent role for acquired factors. Understanding the risks that predispose IBD patients to arterial TE may further elucidate the pathogenesis of thrombosis and potential treatment points. We report a case of a 60yo F with extensive colitis and peripheral arterial thrombosis.
Case Description/Methods: 60-year-old obese female with extensive colitis, previously in remission for over ten years, presented to the emergency department with five day onset of abdominal pain, increased frequency of bowel movements, urgency, nocturnal events, and hematochezia. Her vital signs were within normal limits. Physical exam was notable for diffuse abdominal pain on palpation. Her laboratory studies revealed elevated inflammatory markers: Fecal calprotectin 2092 mcg/g, C-reactive protein 30.65 mg/dL, and white cell count 20.5 x 103/mcL. Stool culture and C. difficile PCR were negative. Abdominal Computed Tomography (CT) showed diffuse pan-colonic wall thickening. No discernible mass noted. She was started on intravenous steroids.
On hospital day 3, she complained of severe right leg pain. Physical exam revealed a mottled, pallorous limb with an absent tibial arterial pulse, concerning for acute limb ischemia. Patient was started on heparin anticoagulation and was evaluated by the vascular surgery team. Emergent angiogram confirmed the diagnosis. She underwent right femoral, popliteal, and tibial arterial thrombectomies. A hypercoagulable work-up by the hematology team was negative. Flexible sigmoidoscopy revealed diffuse large ulcers with biopsies negative for cytomegalovirus. The patient was transitioned to apixaban anticoagulation and oral prednisone taper. Infliximab was started.
Discussion: Peripheral arterial thrombosis is a rare complication in IBD with a reported incidence of less than 1 in 1000. Its pathogenesis is unknown. Our patient risk factors include obesity, gender, disease flare, and hospitalization. This case highlights the presence of arterial thrombosis in IBD and the need for continued case reporting, paramount to guide further investigations.

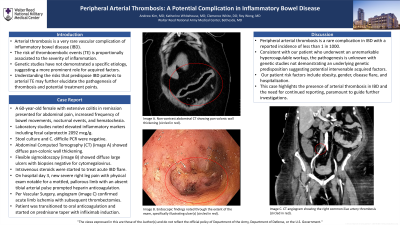
Figure: Image A is a non-contrast abdominal CT showing pancolonic wall thickening (circled in red). Image B is a CT angiogram showing the right common iliac artery thrombosis (circled in red). Image C is the endoscopic findings noted through the extent of the exam, specifically illustrating the ulcer(s) (circled in red).
Disclosures:
Andrew Kim indicated no relevant financial relationships.
Clemence White indicated no relevant financial relationships.
Roy Wong indicated no relevant financial relationships.
Katherine Whitehouse indicated no relevant financial relationships.
Andrew Kim, MD, Clemence C. White, DO, Roy Wong, MD, Katherine M. Whitehouse, MD. P0810 - Peripheral Arterial Thrombosis: A Potential Complication in Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
