Sunday Poster Session
Category: IBD
P0819 - Cloudy Picture With Ozanimod: A Rare Case of S1P Modulator Therapy-Associated Macular Edema
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- CC
Christopher M. Cowan, MD
San Antonio Uniformed Services Health Consortium
Fort Sam Houston, TX
Presenting Author(s)
Christopher M. Cowan, MD1, Anish Patel, DO2
1San Antonio Uniformed Services Health Consortium, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Ulcerative Colitis (UC) is a chronic autoimmune condition predominately manifesting as colonic inflammation with serious morbidity. Early intervention can alter the disease course, improving symptoms and reducing the need for hospitalization and surgery. Multiple new medications have recently been introduced that greatly expand treatment options but also potential idiosyncratic reactions. We present a case of sphingosine-1 phosphate receptor (S1P) modulator therapy (ozanimod) associated macular edema to highlight this rare, serious complication, in the setting of concurrent cataract surgery.
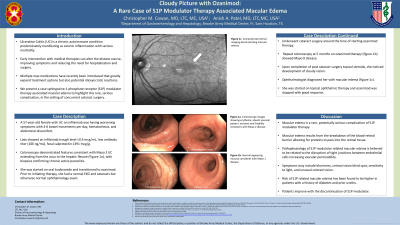
Case Description/Methods: A 57 year-old female with UC on infliximab was following up for worsening symptoms of 4-6 bowel movements per day, hematochezia, and abdominal discomfort. Labs showed trough infliximab level < 0.4 mcg/mL with low antibody titer (106 ng/mL) and fecal calprotectin 1391 mcg/g. She underwent a colonoscopy, which demonstrated features consistent with Mayo 2 UC extending from the anus to hepatic flexure (Figure 1a), with biopsies confirming chronic active pancolitis. Patient was started on oral budesonide and transitioned to ozanimod. Prior to initiating therapy, she had a normal EKG and ophthalmology exam. Underwent cataract surgery around the time of starting ozanimod therapy. Repeat colonoscopy at 5 months on ozanimod therapy (Figure 1b) showed Mayo 0 disease. Upon completion of post cataract surgery topical steroids, she presented with cloudy vision to ophthalmology and was found to have macular edema (Figure 1c). Patient was started on topical ophthalmic therapy and ozanimod was stopped with good response.
Discussion: Macular edema is a rare, potentially serious complication of S1P modulator therapy. Macular edema results from the breakdown of the blood-retinal barrier allowing for proteins to pass into the retinal tissue. The pathophysiology of S1P modulator related macular edema is believed to be related to disruption of the tight junctions between endothelial cells increasing vascular permeability. Symptoms include blurriness, central vision blind spot, sensitivity to light, or unusually colored vision. Risk of S1P related macular edema has been found to be higher in patients with a history of diabetes and prior uveitis. Patients improve with discontinuation of S1P modulator. Our case serves to remind clinicians of this serious side effect, importance of thorough risk-benefits counseling prior to treatment, and potential increased risk with cataract surgery while on S1P therapy.

Disclosures:
Christopher M. Cowan, MD1, Anish Patel, DO2. P0819 - Cloudy Picture With Ozanimod: A Rare Case of S1P Modulator Therapy-Associated Macular Edema, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1San Antonio Uniformed Services Health Consortium, Fort Sam Houston, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Ulcerative Colitis (UC) is a chronic autoimmune condition predominately manifesting as colonic inflammation with serious morbidity. Early intervention can alter the disease course, improving symptoms and reducing the need for hospitalization and surgery. Multiple new medications have recently been introduced that greatly expand treatment options but also potential idiosyncratic reactions. We present a case of sphingosine-1 phosphate receptor (S1P) modulator therapy (ozanimod) associated macular edema to highlight this rare, serious complication, in the setting of concurrent cataract surgery.
Case Description/Methods: A 57 year-old female with UC on infliximab was following up for worsening symptoms of 4-6 bowel movements per day, hematochezia, and abdominal discomfort. Labs showed trough infliximab level < 0.4 mcg/mL with low antibody titer (106 ng/mL) and fecal calprotectin 1391 mcg/g. She underwent a colonoscopy, which demonstrated features consistent with Mayo 2 UC extending from the anus to hepatic flexure (Figure 1a), with biopsies confirming chronic active pancolitis. Patient was started on oral budesonide and transitioned to ozanimod. Prior to initiating therapy, she had a normal EKG and ophthalmology exam. Underwent cataract surgery around the time of starting ozanimod therapy. Repeat colonoscopy at 5 months on ozanimod therapy (Figure 1b) showed Mayo 0 disease. Upon completion of post cataract surgery topical steroids, she presented with cloudy vision to ophthalmology and was found to have macular edema (Figure 1c). Patient was started on topical ophthalmic therapy and ozanimod was stopped with good response.
Discussion: Macular edema is a rare, potentially serious complication of S1P modulator therapy. Macular edema results from the breakdown of the blood-retinal barrier allowing for proteins to pass into the retinal tissue. The pathophysiology of S1P modulator related macular edema is believed to be related to disruption of the tight junctions between endothelial cells increasing vascular permeability. Symptoms include blurriness, central vision blind spot, sensitivity to light, or unusually colored vision. Risk of S1P related macular edema has been found to be higher in patients with a history of diabetes and prior uveitis. Patients improve with discontinuation of S1P modulator. Our case serves to remind clinicians of this serious side effect, importance of thorough risk-benefits counseling prior to treatment, and potential increased risk with cataract surgery while on S1P therapy.

Figure: Figure 1a: Colonoscopy images showing erythema, absent vascular patterns, erosions, and friability consistent with Mayo 2 disease.
Figure 1b: Normal appearing mucosa consistent with Mayo 0 disease.
Fiigure 1c: Computerized retinal imaging demonstrating macular edema.
Figure 1b: Normal appearing mucosa consistent with Mayo 0 disease.
Fiigure 1c: Computerized retinal imaging demonstrating macular edema.
Disclosures:
Christopher Cowan indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Christopher M. Cowan, MD1, Anish Patel, DO2. P0819 - Cloudy Picture With Ozanimod: A Rare Case of S1P Modulator Therapy-Associated Macular Edema, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
