Sunday Poster Session
Category: IBD
P0820 - A Case of mRNA Vaccine-Induced Autoimmunity
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- KH
Kelly Hu, MD
Stanford Health Care
Mountain View, CA
Presenting Author(s)
Kelly Hu, MD1, Nielsen Fernandez-Becker, MD, PhD2
1Stanford Health Care, Mountain View, CA; 2Stanford University, Redwood City, CA
Introduction: Vaccine-induced autoimmunity has been previously described with many protein subunit vaccines. Many mechanisms have been proposed, though it is largely thought to occur via molecular mimicry. In the wake of the COVID-19 pandemic that saw the rapid development and distribution of several new vaccines using novel technology, there are emerging reports of new-onset autoimmune conditions following vaccination with mRNA-based vaccines.
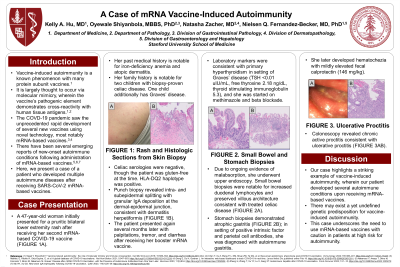
Case Description/Methods: The patient is a 47-year-old woman with a history of iron-deficiency anemia and atopic dermatitis. Her family history is notable for two children with biopsy-proven celiac disease, one of whom additionally has Graves’ disease. She initially presented for an intermittent, pruritic lower extremity rash that developed after her second mRNA-based COVID-19 vaccine. Celiac serologies were negative (she was gluten-free at the time) but her HLA-DQ2 haplotype was positive. Punch biopsy of her rash was notable for intra- and subepidermal splitting with granular IgA deposition at the dermal/epidermal junction, consistent with dermatitis herpetiformis.
Several months later, she received a booster and shortly thereafter, she presented to the emergency room with acute palpitations, tremor, and diarrhea. TSH was undetectable with elevated free T4 and TSI consistent with primary hyperthyroidism in setting of Graves’ disease; she was started on treatment with methimazole and beta blockade. Due to ongoing evidence of malabsorption, she underwent upper endoscopy that was consistent with treated celiac disease (increased duodenal lymphocytes with preserved villous architecture) as well as atrophic gastritis and elevated IF antibody suggestive of autoimmune gastritis. She later developed hematochezia; colonoscopy had evidence of chronic active proctitis, and in conjunction with a mildly elevated fecal calprotectin, she was additionally diagnosed with ulcerative proctitis and started on mesalamine with resolution of symptoms.
Discussion: Our case highlights a striking example of vaccine-induced autoimmunity, wherein the patient developed several new-onset autoimmune conditions, particularly gastrointestinal disorders, upon receiving mRNA-based vaccines. Given only a small subset of patients experience this phenomenon, it suggests there may exist a genetic predisposition for autoimmunity triggered by vaccination. Our case underscores the need to use mRNA-based vaccines with caution in patients at high risk for autoimmunity.

Disclosures:
Kelly Hu, MD1, Nielsen Fernandez-Becker, MD, PhD2. P0820 - A Case of mRNA Vaccine-Induced Autoimmunity, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford Health Care, Mountain View, CA; 2Stanford University, Redwood City, CA
Introduction: Vaccine-induced autoimmunity has been previously described with many protein subunit vaccines. Many mechanisms have been proposed, though it is largely thought to occur via molecular mimicry. In the wake of the COVID-19 pandemic that saw the rapid development and distribution of several new vaccines using novel technology, there are emerging reports of new-onset autoimmune conditions following vaccination with mRNA-based vaccines.
Case Description/Methods: The patient is a 47-year-old woman with a history of iron-deficiency anemia and atopic dermatitis. Her family history is notable for two children with biopsy-proven celiac disease, one of whom additionally has Graves’ disease. She initially presented for an intermittent, pruritic lower extremity rash that developed after her second mRNA-based COVID-19 vaccine. Celiac serologies were negative (she was gluten-free at the time) but her HLA-DQ2 haplotype was positive. Punch biopsy of her rash was notable for intra- and subepidermal splitting with granular IgA deposition at the dermal/epidermal junction, consistent with dermatitis herpetiformis.
Several months later, she received a booster and shortly thereafter, she presented to the emergency room with acute palpitations, tremor, and diarrhea. TSH was undetectable with elevated free T4 and TSI consistent with primary hyperthyroidism in setting of Graves’ disease; she was started on treatment with methimazole and beta blockade. Due to ongoing evidence of malabsorption, she underwent upper endoscopy that was consistent with treated celiac disease (increased duodenal lymphocytes with preserved villous architecture) as well as atrophic gastritis and elevated IF antibody suggestive of autoimmune gastritis. She later developed hematochezia; colonoscopy had evidence of chronic active proctitis, and in conjunction with a mildly elevated fecal calprotectin, she was additionally diagnosed with ulcerative proctitis and started on mesalamine with resolution of symptoms.
Discussion: Our case highlights a striking example of vaccine-induced autoimmunity, wherein the patient developed several new-onset autoimmune conditions, particularly gastrointestinal disorders, upon receiving mRNA-based vaccines. Given only a small subset of patients experience this phenomenon, it suggests there may exist a genetic predisposition for autoimmunity triggered by vaccination. Our case underscores the need to use mRNA-based vaccines with caution in patients at high risk for autoimmunity.

Figure: Figure 1. Bilateral buttocks with scattered erythematous crusted papules and erosions.
Disclosures:
Kelly Hu indicated no relevant financial relationships.
Nielsen Fernandez-Becker indicated no relevant financial relationships.
Kelly Hu, MD1, Nielsen Fernandez-Becker, MD, PhD2. P0820 - A Case of mRNA Vaccine-Induced Autoimmunity, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

