Sunday Poster Session
Category: IBD
P0823 - An Atypical Presentation of Ileocolitis Beyond Inflammatory Bowel Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jacqueline Khalil, DO, MS
Case Western Reserve University/Metro Health
Cleveland, OH
Presenting Author(s)
Jacqueline Khalil, DO, MS1, Marc Landsman, MD2
1Case Western Reserve University/Metro Health, Cleveland, OH; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Ileocolitis is defined as inflammation of the ileum and colon, which is commonly seen in Crohn’s Disease (CD). Distinguishing between the various etiologies of ileocolitis remains a clinical challenge. However, it is important to keep a broad differential to prevent misdiagnosis. Thus, the diagnosis is based on a collection of clinical, laboratory, endoscopic, and histologic data. This case presentation aims to examine these entities and provoke discussion on the underlying etiologies of ileocolitis beyond inflammatory bowel disease (IBD).
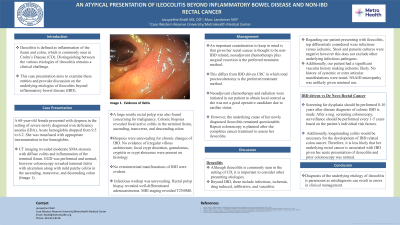
Case Description/Methods: A 60-year-old female presented with dyspnea in the setting of severe newly diagnosed iron deficiency anemia (IDA). Acute hemoglobin dropped from 9.5 to 6.2. She was transfused with appropriate incrementation. CT imaging revealed moderate SMA stenosis. EGD was performed and normal, however colonoscopy revealed terminal ileitis with ulceration along with mild patchy colitis in the ascending, transverse, and descending colon. A large sessile rectal polyp was also found. Colonic biopsies revealed focal active colitis in the terminal ileum, ascending, transverse, and descending colon. Biopsies showed no evidence of IBD. Infectious workup was unrevealing. Rectal biopsy revealed adenocarcinoma. Staging was T2N0. The patient underwent neoadjuvant chemotherapy and radiation. However, the underlying cause of her newly diagnosed ileocolitis remained questionable. Repeat colonoscopy is planned after she completes cancer treatment to assess her ileocolitis.
Discussion: Diagnosis of the underlying etiology of ileocolitis is paramount because misdiagnosis can result in errors in clinical management. Although ileocolitis is commonly seen in the setting of CD, it is important to consider other presenting etiologies. Beyond IBD, these include infectious, ischemia, drug induced, infiltrative, and vasculitis. Regarding our patient presenting with ileocolitis, top differentials considered were infectious versus ischemic. Stool and parasite cultures were negative however this does not exclude other underlying infectious pathogens. Additionally, our patient had a significant vascular history making ischemic likely. No history of systemic or extra articular manifestations were noted. NSAID enteropathy was unlikely given minimal use. Biopsies were unrevealing for IBD. Additionally, longstanding colitis would be necessary for the development of IBD related colon cancer. Therefore, it is less likely that her underlying rectal cancer is associated with IBD.

Disclosures:
Jacqueline Khalil, DO, MS1, Marc Landsman, MD2. P0823 - An Atypical Presentation of Ileocolitis Beyond Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University/Metro Health, Cleveland, OH; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Ileocolitis is defined as inflammation of the ileum and colon, which is commonly seen in Crohn’s Disease (CD). Distinguishing between the various etiologies of ileocolitis remains a clinical challenge. However, it is important to keep a broad differential to prevent misdiagnosis. Thus, the diagnosis is based on a collection of clinical, laboratory, endoscopic, and histologic data. This case presentation aims to examine these entities and provoke discussion on the underlying etiologies of ileocolitis beyond inflammatory bowel disease (IBD).
Case Description/Methods: A 60-year-old female presented with dyspnea in the setting of severe newly diagnosed iron deficiency anemia (IDA). Acute hemoglobin dropped from 9.5 to 6.2. She was transfused with appropriate incrementation. CT imaging revealed moderate SMA stenosis. EGD was performed and normal, however colonoscopy revealed terminal ileitis with ulceration along with mild patchy colitis in the ascending, transverse, and descending colon. A large sessile rectal polyp was also found. Colonic biopsies revealed focal active colitis in the terminal ileum, ascending, transverse, and descending colon. Biopsies showed no evidence of IBD. Infectious workup was unrevealing. Rectal biopsy revealed adenocarcinoma. Staging was T2N0. The patient underwent neoadjuvant chemotherapy and radiation. However, the underlying cause of her newly diagnosed ileocolitis remained questionable. Repeat colonoscopy is planned after she completes cancer treatment to assess her ileocolitis.
Discussion: Diagnosis of the underlying etiology of ileocolitis is paramount because misdiagnosis can result in errors in clinical management. Although ileocolitis is commonly seen in the setting of CD, it is important to consider other presenting etiologies. Beyond IBD, these include infectious, ischemia, drug induced, infiltrative, and vasculitis. Regarding our patient presenting with ileocolitis, top differentials considered were infectious versus ischemic. Stool and parasite cultures were negative however this does not exclude other underlying infectious pathogens. Additionally, our patient had a significant vascular history making ischemic likely. No history of systemic or extra articular manifestations were noted. NSAID enteropathy was unlikely given minimal use. Biopsies were unrevealing for IBD. Additionally, longstanding colitis would be necessary for the development of IBD related colon cancer. Therefore, it is less likely that her underlying rectal cancer is associated with IBD.

Figure: Mild patchy colitis with ulceration
Disclosures:
Jacqueline Khalil indicated no relevant financial relationships.
Marc Landsman indicated no relevant financial relationships.
Jacqueline Khalil, DO, MS1, Marc Landsman, MD2. P0823 - An Atypical Presentation of Ileocolitis Beyond Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
