Sunday Poster Session
Category: IBD
P0825 - A Rare Case of Concurrent Vulvar Crohn’s Disease and Pyoderma Gangrenosum
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jaya Bommireddipally, MD
Tulane University
New Orleans, LA
Presenting Author(s)
Jaya Bommireddipally, MD1, Kent Broussard, MD2, Hanadi Osman, MD3, Ann Uhlhorn, RN4, Nisha Loganantharaj, MD5
1Tulane University, New Orleans, LA; 2Louisiana State University School of Medicine, Metairie, LA; 3Tulane University School of Medicine, New Orleans, LA; 4Louisiana State University, New Orleans, LA; 5Louisiana State University School of Medicine, New Orleans, LA
Introduction: Crohn’s disease (CD) is a chronic inflammatory condition affecting the gastrointestinal tract and can result in extra-intestinal inflammation. Vulvar CD (VCD) is a rare extra-intestinal manifestation of CD with one study reporting VCD in less than 0.25% of women with inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG) is an autoinflammatory dermatitis with neutrophilic dysfunction that has also been infrequently seen in patients with IBD. Coexistent VCD and PG is exceedingly rare with only a few cases reported in the literature.
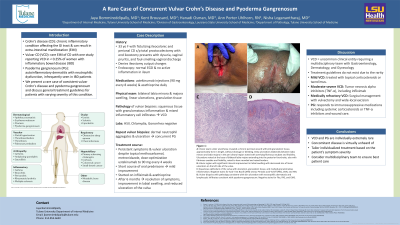
Case Description/Methods: A 33-year-old female with fistulizing ileocolonic and perianal CD status-post total proctocolectomy with end ileostomy presents with dysuria, vaginal pruritis, and foul-smelling vaginal discharge. She denies any changes in her ileostomy output or bleeding from her ostomy. Her medications include ustekinumab injections (90 mg every 8 weeks) and azathioprine daily. Physical exam reveals bilateral labia minora and majora swelling, linear ulcerations, and granulation tissue. Pathology of vulvar biopsies showed squamous tissue with granulomatous inflammation and mixed inflammatory cell infiltrates consistent with VCD. Tests for HSV, Chlamydia, and Gonorrhea were negative. She then had repeat vulvar biopsies with neutrophil aggregates in the dermis and ulceration consistent with concurrent PG (Figure 1). She had persistent symptoms and vulvar ulceration despite therapy with topical methocarbamol, metronidazole, and dose-optimization of her ustekinumab to 90 mg every 4 weeks. She had mild clinical improvement on a short course of oral prednisone but was ultimately started on infliximab and azathioprine. After 6 months of therapy, she had resolution of her symptoms, improvement in labial swelling, and reduced ulceration of the vulva.
Discussion: VCD is an uncommon clinical entity requiring a multidisciplinary team with Gastroenterology, Dermatology, and Gynecology. Treatment guidelines do not exist due to the rarity of the condition, but multiple regimens have been employed. Mild VCD can be treated with topical corticosteroids or tacrolimus. Prior studies recommend the early use of cyclosporine or tumor necrosis alpha inhibitors (TNF-α) including infliximab for moderate-to-severe VCD. Surgical management with vulvectomy and wide-local excision can be considered in medically refractory disease. PG often rapidly responds to immunosuppressive medications including systemic corticosteroids or TNF-α inhibitors and wound care.

Disclosures:
Jaya Bommireddipally, MD1, Kent Broussard, MD2, Hanadi Osman, MD3, Ann Uhlhorn, RN4, Nisha Loganantharaj, MD5. P0825 - A Rare Case of Concurrent Vulvar Crohn’s Disease and Pyoderma Gangrenosum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tulane University, New Orleans, LA; 2Louisiana State University School of Medicine, Metairie, LA; 3Tulane University School of Medicine, New Orleans, LA; 4Louisiana State University, New Orleans, LA; 5Louisiana State University School of Medicine, New Orleans, LA
Introduction: Crohn’s disease (CD) is a chronic inflammatory condition affecting the gastrointestinal tract and can result in extra-intestinal inflammation. Vulvar CD (VCD) is a rare extra-intestinal manifestation of CD with one study reporting VCD in less than 0.25% of women with inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG) is an autoinflammatory dermatitis with neutrophilic dysfunction that has also been infrequently seen in patients with IBD. Coexistent VCD and PG is exceedingly rare with only a few cases reported in the literature.
Case Description/Methods: A 33-year-old female with fistulizing ileocolonic and perianal CD status-post total proctocolectomy with end ileostomy presents with dysuria, vaginal pruritis, and foul-smelling vaginal discharge. She denies any changes in her ileostomy output or bleeding from her ostomy. Her medications include ustekinumab injections (90 mg every 8 weeks) and azathioprine daily. Physical exam reveals bilateral labia minora and majora swelling, linear ulcerations, and granulation tissue. Pathology of vulvar biopsies showed squamous tissue with granulomatous inflammation and mixed inflammatory cell infiltrates consistent with VCD. Tests for HSV, Chlamydia, and Gonorrhea were negative. She then had repeat vulvar biopsies with neutrophil aggregates in the dermis and ulceration consistent with concurrent PG (Figure 1). She had persistent symptoms and vulvar ulceration despite therapy with topical methocarbamol, metronidazole, and dose-optimization of her ustekinumab to 90 mg every 4 weeks. She had mild clinical improvement on a short course of oral prednisone but was ultimately started on infliximab and azathioprine. After 6 months of therapy, she had resolution of her symptoms, improvement in labial swelling, and reduced ulceration of the vulva.
Discussion: VCD is an uncommon clinical entity requiring a multidisciplinary team with Gastroenterology, Dermatology, and Gynecology. Treatment guidelines do not exist due to the rarity of the condition, but multiple regimens have been employed. Mild VCD can be treated with topical corticosteroids or tacrolimus. Prior studies recommend the early use of cyclosporine or tumor necrosis alpha inhibitors (TNF-α) including infliximab for moderate-to-severe VCD. Surgical management with vulvectomy and wide-local excision can be considered in medically refractory disease. PG often rapidly responds to immunosuppressive medications including systemic corticosteroids or TNF-α inhibitors and wound care.

Figure: Figure 1: A: Vulvar exam under anesthesia revealed a chronic perineal wound with pink granulation tissue, approximately 4cm in length, without drainage or bleeding. Deep ulcerations bilaterally between labia minora and labia majora in the peri clitoral region noted with overlying fibrinous exudate and friability. Ulcerations noted at the base of bilateral labia majora extending into the posterior fourchette, also with fibrinous exudate and friability, noted to have rounded and raised borders.
B: Vulvar region with significant interval improvement in labial swelling with decreased size of linear ulceration on the left side of the vulva.
C: Squamous epithelium of the vulva with ulceration, granulation tissue, and marked granulomatous inflammation. Negative stains for Acid- Fast Bacilli (AFB) smear, Periodic acid–Schiff (PAS), CMV, and HSV.
D: Vulvar biopsies with pathology consistent with skin ulceration with neutrophilic dermatosis and lymphocytic infiltrates consistent with pyoderma gangrenosum. Negative stains for Fite, PAS, and GMS.
B: Vulvar region with significant interval improvement in labial swelling with decreased size of linear ulceration on the left side of the vulva.
C: Squamous epithelium of the vulva with ulceration, granulation tissue, and marked granulomatous inflammation. Negative stains for Acid- Fast Bacilli (AFB) smear, Periodic acid–Schiff (PAS), CMV, and HSV.
D: Vulvar biopsies with pathology consistent with skin ulceration with neutrophilic dermatosis and lymphocytic infiltrates consistent with pyoderma gangrenosum. Negative stains for Fite, PAS, and GMS.
Disclosures:
Jaya Bommireddipally indicated no relevant financial relationships.
Kent Broussard indicated no relevant financial relationships.
Hanadi Osman indicated no relevant financial relationships.
Ann Uhlhorn indicated no relevant financial relationships.
Nisha Loganantharaj indicated no relevant financial relationships.
Jaya Bommireddipally, MD1, Kent Broussard, MD2, Hanadi Osman, MD3, Ann Uhlhorn, RN4, Nisha Loganantharaj, MD5. P0825 - A Rare Case of Concurrent Vulvar Crohn’s Disease and Pyoderma Gangrenosum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
