Sunday Poster Session
Category: IBD
P0826 - Necrobiotic Pulmonary Nodules, an Incidental Finding Turned Chief Complaint
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- MY
Matthew Yurkewicz, DO
Sky Ridge Medical Center
Englewood, CO
Presenting Author(s)
Matthew Yurkewicz, DO1, Kelly Schulte, DO, MA2, Jennifer Griffith, MD2
1Sky Ridge Medical Center, Englewood, CO; 2Sky Ridge Medical Center, Lone Tree, CO
Introduction: Up to 50% of patients diagnosed with an inflammatory bowel disease (IBD) will experience an extraintestinal manifestation (EIM) throughout the course of their disease. Pulmonary EIMs are relatively uncommon with necrobiotic pulmonary nodules noted as an increasingly rare EIM observed in IBD. Necrobiotic nodules are sterile cavitating lung nodules that can serve as a nidus for infection. They are often mistaken for infectious, autoimmune, or even malignant pathologies due to their appearance on imaging. We present a unique case of necrobiotic nodules in a young patient with uncontrolled ulcerative colitis (UC).
Case Description/Methods: A 22 year old female with a past medical history significant for uncontrolled UC on vedolizumab and clostridium difficile infection (CDI) presented with hematochezia and shortness of breath on subsequent hospitalizations.
The patient was hospitalized with complaints of abdominal pain and hematochezia. Stool and CDI studies were negative, so the patient was treated with intravenous corticosteroids for a UC flare. Imaging findings incidentally revealed multiple, bilateral, solid pulmonary nodules. After improvement of the hematochezia, the patient was discharged on oral corticosteroids. The patient returned a month later with shortness of breath and dry cough for two weeks. Repeat imaging revealed an interval size increase of the pulmonary nodules, now with central necrosis. Further workup of infectious/fungal pathologies were negative. The patient underwent biopsy of the pulmonary nodules which showed a predominance of histiocytes, lung parenchyma with organizing pneumonia, and chronic interstitial inflammation of which possible etiologies included infectious, collagen vascular disease, or direct associations with IBD. The shortness of breath improved with monitoring and the patient was discharged.
Discussion: The histiocytic predominance of the pulmonary nodule biopsy and evolution in size with central necrosis of the nodules in the setting of IBD are characteristic of the aforementioned necrobiotic nodules. Necrobiotic nodules are often diagnosed in patients with active luminal IBD who present with respiratory complaints. Our case is unique in that the pulmonary nodules were initially diagnosed incidentally, but came to fruition with respiratory distress on an ensuing hospitalization. Necrobiotic nodules often share a parallel disease course with IBD and in most case studies, with successful treatment of the IBD also comes resolution of the necrobiotic nodules.

Disclosures:
Matthew Yurkewicz, DO1, Kelly Schulte, DO, MA2, Jennifer Griffith, MD2. P0826 - Necrobiotic Pulmonary Nodules, an Incidental Finding Turned Chief Complaint, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Sky Ridge Medical Center, Englewood, CO; 2Sky Ridge Medical Center, Lone Tree, CO
Introduction: Up to 50% of patients diagnosed with an inflammatory bowel disease (IBD) will experience an extraintestinal manifestation (EIM) throughout the course of their disease. Pulmonary EIMs are relatively uncommon with necrobiotic pulmonary nodules noted as an increasingly rare EIM observed in IBD. Necrobiotic nodules are sterile cavitating lung nodules that can serve as a nidus for infection. They are often mistaken for infectious, autoimmune, or even malignant pathologies due to their appearance on imaging. We present a unique case of necrobiotic nodules in a young patient with uncontrolled ulcerative colitis (UC).
Case Description/Methods: A 22 year old female with a past medical history significant for uncontrolled UC on vedolizumab and clostridium difficile infection (CDI) presented with hematochezia and shortness of breath on subsequent hospitalizations.
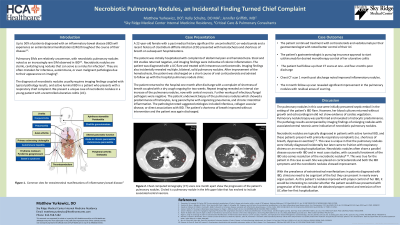
The patient was hospitalized with complaints of abdominal pain and hematochezia. Stool and CDI studies were negative, so the patient was treated with intravenous corticosteroids for a UC flare. Imaging findings incidentally revealed multiple, bilateral, solid pulmonary nodules. After improvement of the hematochezia, the patient was discharged on oral corticosteroids. The patient returned a month later with shortness of breath and dry cough for two weeks. Repeat imaging revealed an interval size increase of the pulmonary nodules, now with central necrosis. Further workup of infectious/fungal pathologies were negative. The patient underwent biopsy of the pulmonary nodules which showed a predominance of histiocytes, lung parenchyma with organizing pneumonia, and chronic interstitial inflammation of which possible etiologies included infectious, collagen vascular disease, or direct associations with IBD. The shortness of breath improved with monitoring and the patient was discharged.
Discussion: The histiocytic predominance of the pulmonary nodule biopsy and evolution in size with central necrosis of the nodules in the setting of IBD are characteristic of the aforementioned necrobiotic nodules. Necrobiotic nodules are often diagnosed in patients with active luminal IBD who present with respiratory complaints. Our case is unique in that the pulmonary nodules were initially diagnosed incidentally, but came to fruition with respiratory distress on an ensuing hospitalization. Necrobiotic nodules often share a parallel disease course with IBD and in most case studies, with successful treatment of the IBD also comes resolution of the necrobiotic nodules.

Figure: Chest computerized tomography (CT) scans one month apart show the progression of the patient's pulmonary nodules. Circled is a pulmonary nodule in the left upper lobe that has evolved to include associated central necrosis.
Disclosures:
Matthew Yurkewicz indicated no relevant financial relationships.
Kelly Schulte indicated no relevant financial relationships.
Jennifer Griffith indicated no relevant financial relationships.
Matthew Yurkewicz, DO1, Kelly Schulte, DO, MA2, Jennifer Griffith, MD2. P0826 - Necrobiotic Pulmonary Nodules, an Incidental Finding Turned Chief Complaint, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

