Sunday Poster Session
Category: Interventional Endoscopy
P0830 - Is Endoscopic Bile Duct Stenting a Risk Factor for Post-ERCP Pancreatitis? A Systematic Review and Meta-Analysis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- FS
Faris Shweikeh, MD
Cleveland Clinic Akron General
Akron, Ohio
Presenting Author(s)
Faris Shweikeh, MD1, Usma Shabir, MD2, Aijaz Sofi, MD1
1Cleveland Clinic Akron General, Akron, OH; 2Digestive Diseases and Surgery Institute, Cleveland Clinic, Cleveland, OH
Introduction: Placement of a stent in the bile duct could potentially block pancreatic duct orifice, which may result in post-ERCP pancreatitis (PEP). Although bile duct stenting is the most commonly performed intervention during ERCP, its association with the development of PEP has been examined less frequently. Additionally, the results of association of PEP with bile duct stenting are inconsistent in these studies. The aim of this meta-analysis is to evaluate the risk of PEP with the placement of biliary stent.
Methods: A literature search of several electronic databases was performed for all the published studies reporting the association of bile duct stenting and PEP. The Inverse Variance method was used to pool data of PEP outcomes in a random effects model. Odds ratio (OR) was used to generate an overall effect estimate of the outcome. Association of PEP with bile duct stenting was calculated separately for pooled univariable OR values as well as pooled multiple-logistic regression OR values. Publication bias was assessed by contour funnel plot and heterogeneity was calculated by I2 test. Methodological quality of the studies was assessed by Newcastle-Ottawa scale.
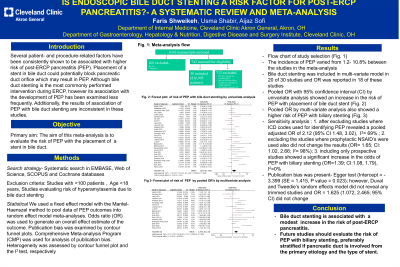
Results: We identified 30 studies (7 prospective and 23 retrospective) with a total of 820,325 patients in the meta-analysis. Of these patients, 205,521 underwent endoscopic biliary stenting. The incidence of PEP varied from 1.2-10.8%. Bile duct stenting was included in multi-variate model in 20 of 30 studies and OR was reported in 18 of these studies. Pooled OR with 95% confidence interval (CI) by univariate analysis showed an increase in the risk of PEP with placement of bile duct stent (OR=1.61;CI:1.06, 2.46), Cochran Q test P< 0.00001. I2=98% (Fig. A). Pooled OR by multi-variate analysis also showed a higher risk of PEP with biliary stenting (Fig. B). Sensitivity analysis was performed after excluding studies where International Statistical Classification of Diseases and related Health Problems (ICD) codes were used for identifying PEP which revealed a pooled adjusted OR of 2.12 (95% CI 1.48, 3.02), Cochran’s Q test P< 0.0001, I2= 69%. Funnel plot appeared asymmetric, however Duval and Tweedie’s random effects model did not reveal any trimmed studies. Only two studies were moderate quality, while other studies were high quality per Newcastle-Ottawa assessment scale.
Discussion: Bile duct stenting is associated with a modest increase in the risk of post-ERCP pancreatitis.

Disclosures:
Faris Shweikeh, MD1, Usma Shabir, MD2, Aijaz Sofi, MD1. P0830 - Is Endoscopic Bile Duct Stenting a Risk Factor for Post-ERCP Pancreatitis? A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Digestive Diseases and Surgery Institute, Cleveland Clinic, Cleveland, OH
Introduction: Placement of a stent in the bile duct could potentially block pancreatic duct orifice, which may result in post-ERCP pancreatitis (PEP). Although bile duct stenting is the most commonly performed intervention during ERCP, its association with the development of PEP has been examined less frequently. Additionally, the results of association of PEP with bile duct stenting are inconsistent in these studies. The aim of this meta-analysis is to evaluate the risk of PEP with the placement of biliary stent.
Methods: A literature search of several electronic databases was performed for all the published studies reporting the association of bile duct stenting and PEP. The Inverse Variance method was used to pool data of PEP outcomes in a random effects model. Odds ratio (OR) was used to generate an overall effect estimate of the outcome. Association of PEP with bile duct stenting was calculated separately for pooled univariable OR values as well as pooled multiple-logistic regression OR values. Publication bias was assessed by contour funnel plot and heterogeneity was calculated by I2 test. Methodological quality of the studies was assessed by Newcastle-Ottawa scale.
Results: We identified 30 studies (7 prospective and 23 retrospective) with a total of 820,325 patients in the meta-analysis. Of these patients, 205,521 underwent endoscopic biliary stenting. The incidence of PEP varied from 1.2-10.8%. Bile duct stenting was included in multi-variate model in 20 of 30 studies and OR was reported in 18 of these studies. Pooled OR with 95% confidence interval (CI) by univariate analysis showed an increase in the risk of PEP with placement of bile duct stent (OR=1.61;CI:1.06, 2.46), Cochran Q test P< 0.00001. I2=98% (Fig. A). Pooled OR by multi-variate analysis also showed a higher risk of PEP with biliary stenting (Fig. B). Sensitivity analysis was performed after excluding studies where International Statistical Classification of Diseases and related Health Problems (ICD) codes were used for identifying PEP which revealed a pooled adjusted OR of 2.12 (95% CI 1.48, 3.02), Cochran’s Q test P< 0.0001, I2= 69%. Funnel plot appeared asymmetric, however Duval and Tweedie’s random effects model did not reveal any trimmed studies. Only two studies were moderate quality, while other studies were high quality per Newcastle-Ottawa assessment scale.
Discussion: Bile duct stenting is associated with a modest increase in the risk of post-ERCP pancreatitis.

Figure: Figure A: Pooled Odds Ratio (OR) with 95% confidence interval (CI) by univariate analysis. Figure B: Pooled OR by multi-variate analysis with corresponding CI.
Disclosures:
Faris Shweikeh indicated no relevant financial relationships.
Usma Shabir indicated no relevant financial relationships.
Aijaz Sofi indicated no relevant financial relationships.
Faris Shweikeh, MD1, Usma Shabir, MD2, Aijaz Sofi, MD1. P0830 - Is Endoscopic Bile Duct Stenting a Risk Factor for Post-ERCP Pancreatitis? A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
