Sunday Poster Session
Category: Interventional Endoscopy
P0838 - Meta-Analysis of Risk Difference in Obstructive Sleep Apnea Before and After Endoscopic Sleeve Gastroplasty
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ellen C. Tan, DO
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Rashmi R. Advani, MD1, Maria Shahzad, 2, Ellen C. Tan, DO3, Kerry Sewell, 4, Hassam Ali, MD5
1Cedars-Sinai Medical Center, Los Angeles, CA; 2University of Health Sciences, Lahore, Punjab, Pakistan; 3OhioHealth Riverside Methodist Hospital, Columbus, OH; 4Laupus Health Sciences Library, East Carolina University, Greenville, NC; 5East Carolina University, Greenville, NC
Introduction: Percentage of weight gain is strongly correlated with risk of obstructive sleep apnea (OSA). Endoscopic sleeve gastroplasty (ESG) has emerged as an important technique to fill the gaps in obesity management amongst lifestyle changes, pharmacotherapy, and bariatric surgery. This is the first meta-analysis on the effects of ESG and improvement of OSA.
Methods: This meta-analysis collated data from studies published from inception to 2023. PubMed Embase (embase.com) and Cochrane CENTRAL (via Ovid) were used to identify studies reporting data on OSA before and after ESG. A total of 1413 results were obtained, with 246 duplicates removed. Among these, 1167 studies were excluded as they did not report ESG and OSA outcomes, and 26 titles were screened via full texts. The final analysis incorporated data from 5 studies that supplied adequate information concerning ESG and OSA. The risk ratio was computed for each study, representing the risk of OSA following ESG. These ratios were pooled using a random-effects pairwise meta-analysis in STATA 16.1 to account for potential heterogeneity between studies, utilizing the DerSimonian-Laird method to estimate between-study variance. The standard errors of these ratios were calculated to assess the precision of the effect estimates. The extent of heterogeneity was quantified and reported using the I² statistic, representing the percentage of total variation across studies due to heterogeneity rather than chance. All analyses were assisted by GPT-4 (Wolfram API).
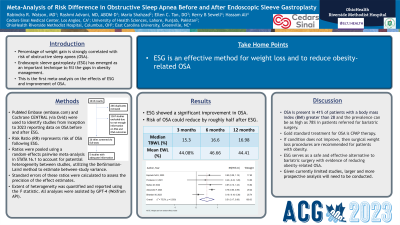
Results: ESG showed a significant improvement in OSA with an overall RR of 0.51 (95% CI [0.17, 0.86], p = 0.004) and moderate heterogeneity (I² = 75.5%), implying that the risk of OSA could reduce by roughly half after ESG (Figure 1). The median TBWL at three months, reported by three studies, was 15.3%. At six months, the median TBWL was 16.6%, as reported by five studies. Six studies reported that by 12 months, the median TBWL was 16.98%. The mean % EWL at three months, as reported by the studies, was 44.08%. Based on the available data, the mean % EWL was 46.66% at six months; finally, at 12 months, the mean % EWL was 44.41%. The high heterogeneity (I² = 75%) underscores the diverse outcomes across the studies. Further research is needed to elucidate the factors contributing to this variability.
Discussion: ESG is an effective method for weight loss and to reduce risk of obesity-related OSA. Given currently limited studies, larger and more prospective analysis will need to be conducted.

Disclosures:
Rashmi R. Advani, MD1, Maria Shahzad, 2, Ellen C. Tan, DO3, Kerry Sewell, 4, Hassam Ali, MD5. P0838 - Meta-Analysis of Risk Difference in Obstructive Sleep Apnea Before and After Endoscopic Sleeve Gastroplasty, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cedars-Sinai Medical Center, Los Angeles, CA; 2University of Health Sciences, Lahore, Punjab, Pakistan; 3OhioHealth Riverside Methodist Hospital, Columbus, OH; 4Laupus Health Sciences Library, East Carolina University, Greenville, NC; 5East Carolina University, Greenville, NC
Introduction: Percentage of weight gain is strongly correlated with risk of obstructive sleep apnea (OSA). Endoscopic sleeve gastroplasty (ESG) has emerged as an important technique to fill the gaps in obesity management amongst lifestyle changes, pharmacotherapy, and bariatric surgery. This is the first meta-analysis on the effects of ESG and improvement of OSA.
Methods: This meta-analysis collated data from studies published from inception to 2023. PubMed Embase (embase.com) and Cochrane CENTRAL (via Ovid) were used to identify studies reporting data on OSA before and after ESG. A total of 1413 results were obtained, with 246 duplicates removed. Among these, 1167 studies were excluded as they did not report ESG and OSA outcomes, and 26 titles were screened via full texts. The final analysis incorporated data from 5 studies that supplied adequate information concerning ESG and OSA. The risk ratio was computed for each study, representing the risk of OSA following ESG. These ratios were pooled using a random-effects pairwise meta-analysis in STATA 16.1 to account for potential heterogeneity between studies, utilizing the DerSimonian-Laird method to estimate between-study variance. The standard errors of these ratios were calculated to assess the precision of the effect estimates. The extent of heterogeneity was quantified and reported using the I² statistic, representing the percentage of total variation across studies due to heterogeneity rather than chance. All analyses were assisted by GPT-4 (Wolfram API).
Results: ESG showed a significant improvement in OSA with an overall RR of 0.51 (95% CI [0.17, 0.86], p = 0.004) and moderate heterogeneity (I² = 75.5%), implying that the risk of OSA could reduce by roughly half after ESG (Figure 1). The median TBWL at three months, reported by three studies, was 15.3%. At six months, the median TBWL was 16.6%, as reported by five studies. Six studies reported that by 12 months, the median TBWL was 16.98%. The mean % EWL at three months, as reported by the studies, was 44.08%. Based on the available data, the mean % EWL was 46.66% at six months; finally, at 12 months, the mean % EWL was 44.41%. The high heterogeneity (I² = 75%) underscores the diverse outcomes across the studies. Further research is needed to elucidate the factors contributing to this variability.
Discussion: ESG is an effective method for weight loss and to reduce risk of obesity-related OSA. Given currently limited studies, larger and more prospective analysis will need to be conducted.

Figure: Forest Plot of 5 Studies
Disclosures:
Rashmi Advani indicated no relevant financial relationships.
Maria Shahzad indicated no relevant financial relationships.
Ellen Tan indicated no relevant financial relationships.
Kerry Sewell indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Rashmi R. Advani, MD1, Maria Shahzad, 2, Ellen C. Tan, DO3, Kerry Sewell, 4, Hassam Ali, MD5. P0838 - Meta-Analysis of Risk Difference in Obstructive Sleep Apnea Before and After Endoscopic Sleeve Gastroplasty, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
