Sunday Poster Session
Category: Interventional Endoscopy
P0846 - Usage of Single Use Duodenoscope Does Not Affect Turnover Time: A Single-center Experience
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Adrian Pona, MD
Prisma Health-Upstate
Greenville, SC
Presenting Author(s)
Adrian Pona, MD1, Varun Moktan, MD1, Diego Lim, MD, MPH1, Wesley Jones, MD2, Veeral M. Oza, MD2
1Prisma Health-Upstate, Greenville, SC; 2Prisma Health, Greenville, SC
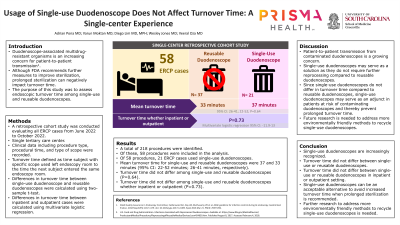
Introduction: Duodenoscope-associated multidrug-resistant organisms and carbapenem-resistant Enterobacteriaceae infections have become an increasing concern for patient-to-patient transmission. To address this, the Food and Drug Administration has recommended further measures to improve sterilization. However, further steps in the sterilization have been shown to not affect transmission rates significantly, and may negatively impact endoscopy room turnover time (TT). Single-use duodenoscopes (SUD) have recently been identified as a potential solution to negate scope associated infection risk. The purpose of this study was to assess the endoscopic TT among SUD and Reusable Duodenoscope (RD).
Methods: After IRB approval, a retrospective cohort study was conducted evaluating all procedures that involved a side-viewing duodenoscope performed over a 2 month period September to October, 2022 at a single tertiary center. Clinical data including procedure type, procedure times including patient in room, patient out of room, and type of scope were recorded. Differences in turnover time between SUD and RD was calculated using a two-sample t-test. Furthermore, a multivariate logistic regression was also performed to record differences in turnover time depending on patient class—inpatient or outpatient. Turnover time was defined as time when patient out of room to the time the next patient in room. Patients where the turnover was impacted by other issues such as intravenous access, or a late patient, or patient out of room delay due to patient status or PACU delays were excluded.
Results: A total of 218 procedures were identified. Of these, 58 procedures were included in the analysis. 21 patients had SUD utilized. Mean TT for SUD and RD was 36.9 minutes (min) versus 33.37 min (95% confidence interval: 21.7-52.1 min vs 25.7-41.1 min, respectively). The endoscopy room TT did not differ regardless of the type of endoscope used (P=0.64). Furthermore, this also remained the case regardless of the patient class—inpatient versus outpatient (P=0.48).
Discussion: Patient-to-patient transmission from contaminated duodenoscopes is a growing concern. SUD may serve as a solution as these do not require further reprocessing. Usage of SUD does not seem to affect TT. This maybe institution specific, and continued data collection at our center over a longer time period are ongoing. Additional collaborative studies including multicenter studies are needed to study this further.
Disclosures:
Adrian Pona, MD1, Varun Moktan, MD1, Diego Lim, MD, MPH1, Wesley Jones, MD2, Veeral M. Oza, MD2. P0846 - Usage of Single Use Duodenoscope Does Not Affect Turnover Time: A Single-center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Prisma Health-Upstate, Greenville, SC; 2Prisma Health, Greenville, SC
Introduction: Duodenoscope-associated multidrug-resistant organisms and carbapenem-resistant Enterobacteriaceae infections have become an increasing concern for patient-to-patient transmission. To address this, the Food and Drug Administration has recommended further measures to improve sterilization. However, further steps in the sterilization have been shown to not affect transmission rates significantly, and may negatively impact endoscopy room turnover time (TT). Single-use duodenoscopes (SUD) have recently been identified as a potential solution to negate scope associated infection risk. The purpose of this study was to assess the endoscopic TT among SUD and Reusable Duodenoscope (RD).
Methods: After IRB approval, a retrospective cohort study was conducted evaluating all procedures that involved a side-viewing duodenoscope performed over a 2 month period September to October, 2022 at a single tertiary center. Clinical data including procedure type, procedure times including patient in room, patient out of room, and type of scope were recorded. Differences in turnover time between SUD and RD was calculated using a two-sample t-test. Furthermore, a multivariate logistic regression was also performed to record differences in turnover time depending on patient class—inpatient or outpatient. Turnover time was defined as time when patient out of room to the time the next patient in room. Patients where the turnover was impacted by other issues such as intravenous access, or a late patient, or patient out of room delay due to patient status or PACU delays were excluded.
Results: A total of 218 procedures were identified. Of these, 58 procedures were included in the analysis. 21 patients had SUD utilized. Mean TT for SUD and RD was 36.9 minutes (min) versus 33.37 min (95% confidence interval: 21.7-52.1 min vs 25.7-41.1 min, respectively). The endoscopy room TT did not differ regardless of the type of endoscope used (P=0.64). Furthermore, this also remained the case regardless of the patient class—inpatient versus outpatient (P=0.48).
Discussion: Patient-to-patient transmission from contaminated duodenoscopes is a growing concern. SUD may serve as a solution as these do not require further reprocessing. Usage of SUD does not seem to affect TT. This maybe institution specific, and continued data collection at our center over a longer time period are ongoing. Additional collaborative studies including multicenter studies are needed to study this further.
Disclosures:
Adrian Pona indicated no relevant financial relationships.
Varun Moktan indicated no relevant financial relationships.
Diego Lim indicated no relevant financial relationships.
Wesley Jones indicated no relevant financial relationships.
Veeral Oza: Boston Scientific – Consultant.
Adrian Pona, MD1, Varun Moktan, MD1, Diego Lim, MD, MPH1, Wesley Jones, MD2, Veeral M. Oza, MD2. P0846 - Usage of Single Use Duodenoscope Does Not Affect Turnover Time: A Single-center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
