Sunday Poster Session
Category: Interventional Endoscopy
P0850 - Safety and Efficacy of Digital Pancreatoscopy via the Minor Papilla for Pancreatic Endotherapy: A Preliminary Experience
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ioannis Pothoulakis, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Ioannis Pothoulakis, MD1, Martin Freeman, MD, MACG2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Pancreatic duct (PD) stones can be associated with significant abdominal pain and decreased quality of life. Management of these stones can be challenging when the PD is difficult to access, such as in cases of pancreas divisum, and might require accessing the PD via the minor papilla instead. We present a case series of patients who underwent ERCP with pancreatoscopy through the minor papilla for pancreatic endotherapy.
Methods: This is a retrospective study of patients who underwent ERCP with minor papilla sphincterotomy and pancreatoscopy at two centers (tertiary care medical center and community based academic center) between 2015 and 2023. Baseline demographics and procedural characteristics were collected from each patient from the electronic medical record. Outcomes included technical success, clinical success, and 30-day adverse events. Technical success was defined as ability to successfully perform digital pancreatoscopy via the minor papilla. Clinical success was defined as complete stone clearance with ERCP. 30-day adverse events included post-ERCP pancreatitis, bleeding, or perforation.
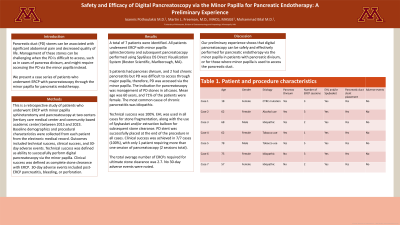
Results: A total of 7 patients were identified. All patients underwent ERCP with minor papilla sphincterotomy and subsequent pancreatoscopy performed using SpyGlass DS Direct Visualization System (Boston Scientific, Marlborough, MA). 5 patients had pancreas divisum, and 2 had chronic pancreatitis but PD was difficult to access through major papilla, therefore, PD was accessed via the minor papilla. The indication for pancreatoscopy was management of PD stones in all cases. Mean age was 60 years, and 71% of the patients were female. The most common cause of chronic pancreatitis was idiopathic. Technical success was 100%. EHL was used in all cases for stone fragmentation, along with the use of Spybasket and/or extraction balloon for subsequent stone clearance. PD stent was successfully placed at the end of the procedure in all cases. Clinical success was achieved in 7/7 cases (100%), with only 1 patient requiring more than one session of pancreatoscopy (2 sessions total). The average number of ERCPs required for ultimate stone clearance was 2.7. No 30-day adverse events were noted.
Discussion: Our preliminary experience shows that digital pancreatoscopy can be safely and effectively performed for pancreatic endotherapy via the minor papilla in patients with pancreatic divisum, or for those where minor papilla is used to access the pancreatic duct.
Disclosures:
Ioannis Pothoulakis, MD1, Martin Freeman, MD, MACG2, Mohammad Bilal, MD3. P0850 - Safety and Efficacy of Digital Pancreatoscopy via the Minor Papilla for Pancreatic Endotherapy: A Preliminary Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Pancreatic duct (PD) stones can be associated with significant abdominal pain and decreased quality of life. Management of these stones can be challenging when the PD is difficult to access, such as in cases of pancreas divisum, and might require accessing the PD via the minor papilla instead. We present a case series of patients who underwent ERCP with pancreatoscopy through the minor papilla for pancreatic endotherapy.
Methods: This is a retrospective study of patients who underwent ERCP with minor papilla sphincterotomy and pancreatoscopy at two centers (tertiary care medical center and community based academic center) between 2015 and 2023. Baseline demographics and procedural characteristics were collected from each patient from the electronic medical record. Outcomes included technical success, clinical success, and 30-day adverse events. Technical success was defined as ability to successfully perform digital pancreatoscopy via the minor papilla. Clinical success was defined as complete stone clearance with ERCP. 30-day adverse events included post-ERCP pancreatitis, bleeding, or perforation.
Results: A total of 7 patients were identified. All patients underwent ERCP with minor papilla sphincterotomy and subsequent pancreatoscopy performed using SpyGlass DS Direct Visualization System (Boston Scientific, Marlborough, MA). 5 patients had pancreas divisum, and 2 had chronic pancreatitis but PD was difficult to access through major papilla, therefore, PD was accessed via the minor papilla. The indication for pancreatoscopy was management of PD stones in all cases. Mean age was 60 years, and 71% of the patients were female. The most common cause of chronic pancreatitis was idiopathic. Technical success was 100%. EHL was used in all cases for stone fragmentation, along with the use of Spybasket and/or extraction balloon for subsequent stone clearance. PD stent was successfully placed at the end of the procedure in all cases. Clinical success was achieved in 7/7 cases (100%), with only 1 patient requiring more than one session of pancreatoscopy (2 sessions total). The average number of ERCPs required for ultimate stone clearance was 2.7. No 30-day adverse events were noted.
Discussion: Our preliminary experience shows that digital pancreatoscopy can be safely and effectively performed for pancreatic endotherapy via the minor papilla in patients with pancreatic divisum, or for those where minor papilla is used to access the pancreatic duct.
Disclosures:
Ioannis Pothoulakis indicated no relevant financial relationships.
Martin Freeman indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant.
Ioannis Pothoulakis, MD1, Martin Freeman, MD, MACG2, Mohammad Bilal, MD3. P0850 - Safety and Efficacy of Digital Pancreatoscopy via the Minor Papilla for Pancreatic Endotherapy: A Preliminary Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
