Sunday Poster Session
Category: Interventional Endoscopy
P0860 - Endoscopic Submucosal Dissection of Gastrointestinal Superficial Neoplastic Lesions: A Canadian Single Center Experience
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Frances Dang, MD, MSc
University of Toronto
Toronto, ON, Canada
Presenting Author(s)
Frances Dang, MD, MSc1, Yusuke Fujiyoshi, MD, MSc1, Suqing Li, MD, MSc2, Gary May, MD1, Jeffrey Mosko, MD, MSc1, Christopher Teshima, MD, PhD1
1University of Toronto, Toronto, ON, Canada; 2University of Calgary, Calgary, AB, Canada
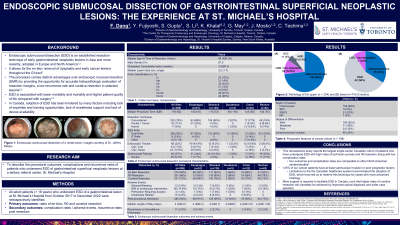
Introduction: Endoscopic submucosal dissection (ESD) is an established resection technique of early gastrointestinal neoplastic lesions. However, the uptake of ESD was delayed in Canada relative to global trends due to a number of challenges within our healthcare system, which include lack of anesthesia support, delayed introduction of ESD devices, limited technical expertise and training opportunities and lack of reimbursement. Here we describe a single tertiary referral center’s experience in adopting ESD to clinical practice in Canada.
Methods: All adult patients ( >18 years) who underwent ESD of a gastrointestinal lesion at St. Michael’s Hospital from October 2017 to December 2021 were retrospectively identified. Primary outcomes were rates of en-bloc, R0 and curative resection. Secondary outcomes included complication rates and recurrence rates post resection.
Results: 203 patients (median age 69 years; 68% were men) underwent ESD (median lesion size 3.0 cm, IQR 1.8 - 4.0) for lesions in the esophagus (n=48), stomach (n=110), duodenum (n=2), colon (n=10) and rectum (n=32). Technical success was 92% for en-bloc resection, 90% for R0 and 77% for curative resection in all patients. Median procedure time was 120 minutes (IQR 92). 95% of cases were admitted to hospital with median length of stay of 4 days (range 1-20). Major post-procedure bleeding occurred in 4% (8/203) and deep mural injury with perforation occurred in 6% (12/203). Pathology revealed 60% (124/203) of lesions were adenocarcinoma with invasion depth characterized as 64% intramucosal (80/124), 13% (17/124) SM1, 19% (24/124) SM2-SM3 and 2% (3/124) muscularis propria. Overall recurrence rate was 3% (6/203) at a mean follow-up time of 249 days(IQR 89 - 334).
Discussion: This study reports the largest single-center Canadian cohort of patients who have undergone ESD with high rates of technical success and R0 resection along with low complication rates. However, limitations specific to the Canadian health care system that have hindered the adoption of ESD have led us to take on many cases with more advanced histology, with more than one-third of our cancer patients having at least submucosal invasion. Our resource limitations mean that earlier stage lesions are still predominantly treated by EMR. We hope that our data helps to sustain the argument that more support is required to facilitate ESD in Canada, such that higher rates of curative resection will ultimately be achieved by allowing more widespread case selection.
Disclosures:
Frances Dang, MD, MSc1, Yusuke Fujiyoshi, MD, MSc1, Suqing Li, MD, MSc2, Gary May, MD1, Jeffrey Mosko, MD, MSc1, Christopher Teshima, MD, PhD1. P0860 - Endoscopic Submucosal Dissection of Gastrointestinal Superficial Neoplastic Lesions: A Canadian Single Center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Toronto, Toronto, ON, Canada; 2University of Calgary, Calgary, AB, Canada
Introduction: Endoscopic submucosal dissection (ESD) is an established resection technique of early gastrointestinal neoplastic lesions. However, the uptake of ESD was delayed in Canada relative to global trends due to a number of challenges within our healthcare system, which include lack of anesthesia support, delayed introduction of ESD devices, limited technical expertise and training opportunities and lack of reimbursement. Here we describe a single tertiary referral center’s experience in adopting ESD to clinical practice in Canada.
Methods: All adult patients ( >18 years) who underwent ESD of a gastrointestinal lesion at St. Michael’s Hospital from October 2017 to December 2021 were retrospectively identified. Primary outcomes were rates of en-bloc, R0 and curative resection. Secondary outcomes included complication rates and recurrence rates post resection.
Results: 203 patients (median age 69 years; 68% were men) underwent ESD (median lesion size 3.0 cm, IQR 1.8 - 4.0) for lesions in the esophagus (n=48), stomach (n=110), duodenum (n=2), colon (n=10) and rectum (n=32). Technical success was 92% for en-bloc resection, 90% for R0 and 77% for curative resection in all patients. Median procedure time was 120 minutes (IQR 92). 95% of cases were admitted to hospital with median length of stay of 4 days (range 1-20). Major post-procedure bleeding occurred in 4% (8/203) and deep mural injury with perforation occurred in 6% (12/203). Pathology revealed 60% (124/203) of lesions were adenocarcinoma with invasion depth characterized as 64% intramucosal (80/124), 13% (17/124) SM1, 19% (24/124) SM2-SM3 and 2% (3/124) muscularis propria. Overall recurrence rate was 3% (6/203) at a mean follow-up time of 249 days(IQR 89 - 334).
Discussion: This study reports the largest single-center Canadian cohort of patients who have undergone ESD with high rates of technical success and R0 resection along with low complication rates. However, limitations specific to the Canadian health care system that have hindered the adoption of ESD have led us to take on many cases with more advanced histology, with more than one-third of our cancer patients having at least submucosal invasion. Our resource limitations mean that earlier stage lesions are still predominantly treated by EMR. We hope that our data helps to sustain the argument that more support is required to facilitate ESD in Canada, such that higher rates of curative resection will ultimately be achieved by allowing more widespread case selection.
Disclosures:
Frances Dang indicated no relevant financial relationships.
Yusuke Fujiyoshi indicated no relevant financial relationships.
Suqing Li indicated no relevant financial relationships.
Gary May indicated no relevant financial relationships.
Jeffrey Mosko indicated no relevant financial relationships.
Christopher Teshima indicated no relevant financial relationships.
Frances Dang, MD, MSc1, Yusuke Fujiyoshi, MD, MSc1, Suqing Li, MD, MSc2, Gary May, MD1, Jeffrey Mosko, MD, MSc1, Christopher Teshima, MD, PhD1. P0860 - Endoscopic Submucosal Dissection of Gastrointestinal Superficial Neoplastic Lesions: A Canadian Single Center Experience, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
