Sunday Poster Session
Category: Interventional Endoscopy
P0862 - Early and Delayed Hemobilia Secondary to Biliary Stenting
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Bharat B. Hans, MD, MSc
NYU Long Island
West Miami, FL
Presenting Author(s)
Bharat Hans, MD, MSc1, Umair Nasir, DO2
1NYU Long Island, Mineola, NY; 2NYU Langone, Mineola, NY
Introduction: Hemobilia (HB) is a rare cause of upper gastrointestinal bleeding (UGIB) resulting from a fistulous connection between hepatic vasculature and the biliary duct. With the advent and rise of advanced endoscopic techniques, we are seeing an increase in the incidence of HB, which commonly presents as a post-ERCP complication. We report a series of two cases where biliary manipulation and stent placement led to either an early (case 1) or delayed (case 2) injury to the hepatic artery resulting in severe HB due to formation of hepatic artery dissection or hepatic pseudoaneurysm (HPA).
Case Description/Methods: Case 1: 24-year-old female presented with choledocholithiasis and dilated common bile duct (CBD) to 1.2 cm. She underwent placement of a 4 Fr 3 cm pancreatic stent into the ventral pancreatic duct and a 7 Fr 7 cm plastic stent into the common bile duct. There was no post-sphincterotomy bleeding noted. Post-op day 1, the patient became hypotensive with a 6-gram drop in hemoglobin and up-trending transaminase levels. CT revealed hepatic hematoma with contrast extravasation in the region of the right hepatic artery. Angiogram revealed hepatic artery dissection, and the patient underwent IR coil embolization. She recovered well, and ERCP was repeated 6 weeks later for stent extraction, lithotripsy, and balloon extraction of stones/sludge.
Case 2: A 69-year-old male with a history of alcoholic pancreatitis presented with emesis and abdominal pain. Imaging showed CBD dilatation without evidence of HPA. ERCP revealed CBD stricture, prompting placement of two 10 Fr 9 cm plastic stents in the CBD. Five months later, he returned with two days of hematemesis. ERCP revealed HB. Extraction of the first stent resulted in brisk, bright red blood from the ampulla. A new stent was placed to tamponade the bleeding. CTA revealed appropriately placed biliary stents adjacent to a right HPA. The patient underwent embolization of HPA with the IR team. Two months later he presented again with hematemesis 1 week later. Fluoroscopy revealed expansion of the right HPA with adjacent biliary stents. The patient underwent repeat coil embolization. Two months later, both plastic stents were extracted without replacement, and CBD stricture was managed with sphincterotomy and dilation.
Discussion: These cases demonstrate how biliary manipulation can lead to early or delayed hemobilia, which should be recognized promptly and considered in the differential diagnosis in post-ERCP patients presenting with signs of GI hemorrhage.

Disclosures:
Bharat Hans, MD, MSc1, Umair Nasir, DO2. P0862 - Early and Delayed Hemobilia Secondary to Biliary Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Long Island, Mineola, NY; 2NYU Langone, Mineola, NY
Introduction: Hemobilia (HB) is a rare cause of upper gastrointestinal bleeding (UGIB) resulting from a fistulous connection between hepatic vasculature and the biliary duct. With the advent and rise of advanced endoscopic techniques, we are seeing an increase in the incidence of HB, which commonly presents as a post-ERCP complication. We report a series of two cases where biliary manipulation and stent placement led to either an early (case 1) or delayed (case 2) injury to the hepatic artery resulting in severe HB due to formation of hepatic artery dissection or hepatic pseudoaneurysm (HPA).
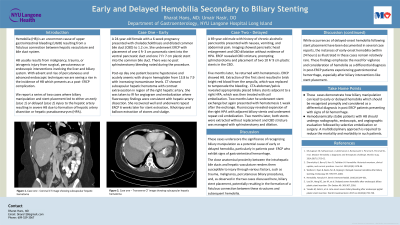
Case Description/Methods: Case 1: 24-year-old female presented with choledocholithiasis and dilated common bile duct (CBD) to 1.2 cm. She underwent placement of a 4 Fr 3 cm pancreatic stent into the ventral pancreatic duct and a 7 Fr 7 cm plastic stent into the common bile duct. There was no post-sphincterotomy bleeding noted. Post-op day 1, the patient became hypotensive with a 6-gram drop in hemoglobin and up-trending transaminase levels. CT revealed hepatic hematoma with contrast extravasation in the region of the right hepatic artery. Angiogram revealed hepatic artery dissection, and the patient underwent IR coil embolization. She recovered well, and ERCP was repeated 6 weeks later for stent extraction, lithotripsy, and balloon extraction of stones/sludge.
Case 2: A 69-year-old male with a history of alcoholic pancreatitis presented with emesis and abdominal pain. Imaging showed CBD dilatation without evidence of HPA. ERCP revealed CBD stricture, prompting placement of two 10 Fr 9 cm plastic stents in the CBD. Five months later, he returned with two days of hematemesis. ERCP revealed HB. Extraction of the first stent resulted in brisk, bright red blood from the ampulla. A new stent was placed to tamponade the bleeding. CTA revealed appropriately placed biliary stents adjacent to a right HPA. The patient underwent embolization of HPA with the IR team. Two months later he presented again with hematemesis 1 week later. Fluoroscopy revealed expansion of the right HPA with adjacent biliary stents. The patient underwent repeat coil embolization. Two months later, both plastic stents were extracted without replacement, and CBD stricture was managed with sphincterotomy and dilation.
Discussion: These cases demonstrate how biliary manipulation can lead to early or delayed hemobilia, which should be recognized promptly and considered in the differential diagnosis in post-ERCP patients presenting with signs of GI hemorrhage.

Figure: Figure 1. CT showing subcapsular hepatic hematoma in patient POD 1 after biliary stent placement.
Disclosures:
Bharat Hans indicated no relevant financial relationships.
Umair Nasir indicated no relevant financial relationships.
Bharat Hans, MD, MSc1, Umair Nasir, DO2. P0862 - Early and Delayed Hemobilia Secondary to Biliary Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
