Sunday Poster Session
Category: Interventional Endoscopy
P0863 - Bridging the Gap: Modified Rendezvous for Treatment of a Bile Duct Injury: A Case Report
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Ryan Kozloski, MD
Womack Army Medical Center
Fort Bragg, North Carolina
Presenting Author(s)
Ryan Kozloski, MD1, Guy S. Dooley, DO2
1Womack Army Medical Center, Fort Bragg, NC; 2Womack Army Medical Center, Southern Pines, NC
Introduction: Common Bile duct injury is a feared complication of laparoscopic cholecystectomy. More and more, these injuries can be repaired via endoscopic retrograde cholangiopancreatography (ERCP), though some injuries require hepatobiliary surgery due to aberrant anatomy or severity of injury. One technique that has helped expand the role of ERCP in treating bile duct injury is the rendezvous procedure. There is growing literature describing various techniques by which rendezvous procedures can be undertaken, which has shown relatively good success with these procedures. 1-3 In this case, we describe a novel variation a rendezvous procedure, which allowed treatment of a complexed bile duct injury, thereby preventing the need for surgical intervention.
Case Description/Methods: In this case, we present an 18-year-old female who underwent laparoscopic cholecystectomy for biliary dyskinesia, who returned to the hospital one month later with nausea, vomiting, and abdominal pain. CT revealed intrahepatic ductal dilation as well as a fluid collection in the gallbladder fossa. Follow-up MRCP confirmed a 3.7 x 3.2 cm fluid collection in the gallbladder fossa. The patient underwent ERCP, confirming a bile duct injury and a bile leak with subsequent biloma formation. Attempts to obtain endoscopic wire guided access across the bile duct injury were unsuccessful as the degree of injury resulted in the guidewire only accessing the biloma. Percutaneous access by interventional radiology was then attempted but was also unable bridge the bile duct injury from an anterograde fashion. Given the inability to stent across the bile duct injury from an anterograde and retrograde approach, a modified rendezvous procedure was performed. A guidewire was passed into the biloma via ERCP and was captured within the biloma by a snare deployed by the interventional radiologist using a trans hepatic approach. This allowed the defect to be effectively bridged, and a stent to be deployed.
Discussion: This case demonstrates a novel procedure to deal with a complex bile duct injury, in which established techniques were deployed in an innovative way to prevent the need for a procedure which carries significant morbidity.

Disclosures:
Ryan Kozloski, MD1, Guy S. Dooley, DO2. P0863 - Bridging the Gap: Modified Rendezvous for Treatment of a Bile Duct Injury: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Womack Army Medical Center, Fort Bragg, NC; 2Womack Army Medical Center, Southern Pines, NC
Introduction: Common Bile duct injury is a feared complication of laparoscopic cholecystectomy. More and more, these injuries can be repaired via endoscopic retrograde cholangiopancreatography (ERCP), though some injuries require hepatobiliary surgery due to aberrant anatomy or severity of injury. One technique that has helped expand the role of ERCP in treating bile duct injury is the rendezvous procedure. There is growing literature describing various techniques by which rendezvous procedures can be undertaken, which has shown relatively good success with these procedures. 1-3 In this case, we describe a novel variation a rendezvous procedure, which allowed treatment of a complexed bile duct injury, thereby preventing the need for surgical intervention.
Case Description/Methods: In this case, we present an 18-year-old female who underwent laparoscopic cholecystectomy for biliary dyskinesia, who returned to the hospital one month later with nausea, vomiting, and abdominal pain. CT revealed intrahepatic ductal dilation as well as a fluid collection in the gallbladder fossa. Follow-up MRCP confirmed a 3.7 x 3.2 cm fluid collection in the gallbladder fossa. The patient underwent ERCP, confirming a bile duct injury and a bile leak with subsequent biloma formation. Attempts to obtain endoscopic wire guided access across the bile duct injury were unsuccessful as the degree of injury resulted in the guidewire only accessing the biloma. Percutaneous access by interventional radiology was then attempted but was also unable bridge the bile duct injury from an anterograde fashion. Given the inability to stent across the bile duct injury from an anterograde and retrograde approach, a modified rendezvous procedure was performed. A guidewire was passed into the biloma via ERCP and was captured within the biloma by a snare deployed by the interventional radiologist using a trans hepatic approach. This allowed the defect to be effectively bridged, and a stent to be deployed.
Discussion: This case demonstrates a novel procedure to deal with a complex bile duct injury, in which established techniques were deployed in an innovative way to prevent the need for a procedure which carries significant morbidity.

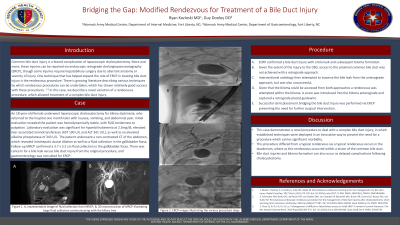
Figure: Images from EGD demonstrating the contrast-filled biloma, with wire coiling, as well as access from the anterior grade/transhepatic approach and final stent placement.
Disclosures:
Ryan Kozloski indicated no relevant financial relationships.
Guy Dooley indicated no relevant financial relationships.
Ryan Kozloski, MD1, Guy S. Dooley, DO2. P0863 - Bridging the Gap: Modified Rendezvous for Treatment of a Bile Duct Injury: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
