Sunday Poster Session
Category: Interventional Endoscopy
P0864 - Rectal EUS-FNB in the Evaluation of Recurrent Endometroid Adenocarcinoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- GK
Grace E. Kim, MD
University of Chicago
Chicago, IL
Presenting Author(s)
Grace Kim, MD1, David Y. Lo, MD, FACG2
1University of Chicago, Chicago, IL; 2Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: Endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) is a standard diagnostic tool for gastrointestinal malignancies. However, inadequate sampling may require further workups. EUS-guided fine needle biopsy (FNB) with tissue acquisition has shown promising results with safety and efficacy in diagnosing various lesions. Here we describe a unique case of diagnosing an incidental subepithelial rectal mass seen on screening colonoscopy with rectal EUS-FNB.
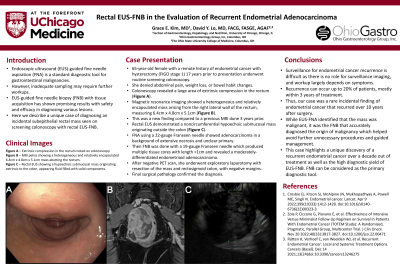
Case Description/Methods: 65-year-old female with a remote history of endometrial cancer with hysterectomy (FIGO stage 1) 17 years ago underwent routine screening colonoscopy. She denied abdominal pain, weight loss, or bowel habit changes. Colonoscopy revealed a large area of extrinsic compression in the rectum (A). Magnetic resonance imaging showed a heterogeneous and relatively encapsulated mass arising from the right lateral wall of the rectum, measuring 6.4cm x 4.8cm x 5.1cm (B). This was a new finding compared to a previous MRI done 3 years prior. Rectal EUS demonstrated a noncircumferential hypoechoic submucosal mass originating outside the colon (C). FNA using a 22-gauge Franseen needle showed adenocarcinoma in a background of extensive necrosis and unclear primary. However, FNB with a 19-gauge Franseen needle produced multiple tissue cores with length >1cm, and revealed a moderately-differentiated endometrioid adenocarcinoma with intact DNA mismatch repair. After negative PET scan, she underwent exploratory laparotomy with resection of the mass and rectosigmoid colon, with negative margins. Final surgical pathology confirmed the diagnosis.
Discussion: Surveillance for endometrial cancer recurrence is difficult as there is no role for surveillance imaging, and workup largely depends on symptoms. One study did not find survival benefit in patients undergoing intensive follow-ups after treatment, even if the patients were at high risk of recurrence. Recurrence can occur up to 20% of patients, mostly within 3 years of treatment. Thus, our case was a rare incidental finding of endometrial cancer that recurred over 10 years after surgery. While EUS-FNA identified that the mass was malignant, it was the FNB that accurately diagnosed the origin of malignancy which helped avoid further unnecessary procedures and guided management. This case highlights a unique discovery of a recurrent endometrial cancer over a decade out of treatment as well as the high diagnostic yield of EUS-FNB. FNB can be considered as the primary diagnostic tool.

Disclosures:
Grace Kim, MD1, David Y. Lo, MD, FACG2. P0864 - Rectal EUS-FNB in the Evaluation of Recurrent Endometroid Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago, Chicago, IL; 2Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: Endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) is a standard diagnostic tool for gastrointestinal malignancies. However, inadequate sampling may require further workups. EUS-guided fine needle biopsy (FNB) with tissue acquisition has shown promising results with safety and efficacy in diagnosing various lesions. Here we describe a unique case of diagnosing an incidental subepithelial rectal mass seen on screening colonoscopy with rectal EUS-FNB.
Case Description/Methods: 65-year-old female with a remote history of endometrial cancer with hysterectomy (FIGO stage 1) 17 years ago underwent routine screening colonoscopy. She denied abdominal pain, weight loss, or bowel habit changes. Colonoscopy revealed a large area of extrinsic compression in the rectum (A). Magnetic resonance imaging showed a heterogeneous and relatively encapsulated mass arising from the right lateral wall of the rectum, measuring 6.4cm x 4.8cm x 5.1cm (B). This was a new finding compared to a previous MRI done 3 years prior. Rectal EUS demonstrated a noncircumferential hypoechoic submucosal mass originating outside the colon (C). FNA using a 22-gauge Franseen needle showed adenocarcinoma in a background of extensive necrosis and unclear primary. However, FNB with a 19-gauge Franseen needle produced multiple tissue cores with length >1cm, and revealed a moderately-differentiated endometrioid adenocarcinoma with intact DNA mismatch repair. After negative PET scan, she underwent exploratory laparotomy with resection of the mass and rectosigmoid colon, with negative margins. Final surgical pathology confirmed the diagnosis.
Discussion: Surveillance for endometrial cancer recurrence is difficult as there is no role for surveillance imaging, and workup largely depends on symptoms. One study did not find survival benefit in patients undergoing intensive follow-ups after treatment, even if the patients were at high risk of recurrence. Recurrence can occur up to 20% of patients, mostly within 3 years of treatment. Thus, our case was a rare incidental finding of endometrial cancer that recurred over 10 years after surgery. While EUS-FNA identified that the mass was malignant, it was the FNB that accurately diagnosed the origin of malignancy which helped avoid further unnecessary procedures and guided management. This case highlights a unique discovery of a recurrent endometrial cancer over a decade out of treatment as well as the high diagnostic yield of EUS-FNB. FNB can be considered as the primary diagnostic tool.

Figure: Figure 1a – external compression in the rectum noted on colonoscopy.
Figure 1b – MRI pelvis showing a heterogeneous and relatively encapsulated mass with lobulated margins arising from the right lateral wall of the mid to lower rectum, likely submucosal/subserosal in location; measures 6.4cm x 4.8xm x 5.1cm
Figure 1c – rectal EUS showing a 2.2 x 4.7cm hypoechoic submucosal mass originating outside the colon, appearing fluid filled with solid components
Figure 1b – MRI pelvis showing a heterogeneous and relatively encapsulated mass with lobulated margins arising from the right lateral wall of the mid to lower rectum, likely submucosal/subserosal in location; measures 6.4cm x 4.8xm x 5.1cm
Figure 1c – rectal EUS showing a 2.2 x 4.7cm hypoechoic submucosal mass originating outside the colon, appearing fluid filled with solid components
Disclosures:
Grace Kim indicated no relevant financial relationships.
David Lo indicated no relevant financial relationships.
Grace Kim, MD1, David Y. Lo, MD, FACG2. P0864 - Rectal EUS-FNB in the Evaluation of Recurrent Endometroid Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
