Sunday Poster Session
Category: Interventional Endoscopy
P0867 - Management of a Necrotic Pancreatic Pseudocyst – Avoiding the Dreaded Pseudoaneurysm Bleed
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ahila Manivannan, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Ahila Manivannan, MD1, William Davis, DO2, Stephanie Betcher, MD1, Robert Pompa, MD2
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Hemorrhagic pancreatic pseudocysts are rare but potentially fatal complication of pancreatitis, often from the development of pseudoaneurysms. We report a case of a large necrotic pancreatic pseudocyst complicated by a pseudoaneurysm bleed, which highlights the importance of thorough evaluation by endoscopic ultrasound (EUS) before therapeutic intervention.
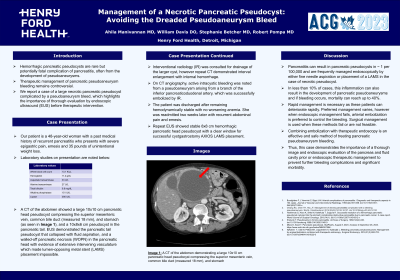
Case Description/Methods: Our patient is a 48-year-old woman with a past medical history of recurrent pancreatitis who presents with severe epigastric pain, emesis and 35 pounds of unintentional weight loss. Laboratory studies demonstrated white blood cell count of 13.1 K/uL, AST 33 U/L, ALT 27 U/L, total bilirubin 0.8 mg/dL, alkaline phosphatase 151 IU/L, lipase 395 IU/L. Computed Tomography (CT) abdomen showed a large 10x10 cm pancreatic head pseudocyst compressing the superior mesenteric vein, common bile duct (measured 18 mm), and stomach (seen in figure 1), and a 10x8x6 cm pseudocyst in the pancreatic tail. EUS demonstrated the pancreatic tail pseudocyst that collapsed with fluid aspiration, and a walled-off pancreatic necrosis (WOPN) in the pancreatic head with evidence of extensive intervening vasculature which made lumen-apposing metal stent (LAMS) stent placement impossible. Interventional radiology (IR) was consulted for drainage of the larger cyst, however repeat CT demonstrated interval enlargement with internal hemorrhage. On CT angiography, active intracystic bleeding was noted from a pseudoaneurysm arising from a branch of the inferior pancreaticoduodenal artery, which was successfully embolized by IR. The patient was discharged after remaining hemodynamically stable with no worsening anemia. She was readmitted two weeks later with recurrent abdominal pain and emesis. Repeat EUS showed stable 8x8 cm hemorrhagic pancreatic head pseudocyst with a clear window for successful cystgastrostomy AXIOS LAMS placement.
Discussion: Pancreatitis can result in pancreatic pseudocysts in ~ 1 per 100,000 and are frequently managed endoscopically by either fine needle aspiration or placement of a LAMS in the case of necrotic pseudocyst. In less than 10% of cases, this inflammation can also result in the development of pancreatic pseudoaneurysms, and if bleeding occurs, mortality can reach up to 40%. Thus, this case demonstrates the importance of thorough imaging and endoscopic evaluation of the pancreas and fluid cavity prior to endoscopic therapeutic management to prevent further bleeding complications.

Disclosures:
Ahila Manivannan, MD1, William Davis, DO2, Stephanie Betcher, MD1, Robert Pompa, MD2. P0867 - Management of a Necrotic Pancreatic Pseudocyst – Avoiding the Dreaded Pseudoaneurysm Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Hemorrhagic pancreatic pseudocysts are rare but potentially fatal complication of pancreatitis, often from the development of pseudoaneurysms. We report a case of a large necrotic pancreatic pseudocyst complicated by a pseudoaneurysm bleed, which highlights the importance of thorough evaluation by endoscopic ultrasound (EUS) before therapeutic intervention.
Case Description/Methods: Our patient is a 48-year-old woman with a past medical history of recurrent pancreatitis who presents with severe epigastric pain, emesis and 35 pounds of unintentional weight loss. Laboratory studies demonstrated white blood cell count of 13.1 K/uL, AST 33 U/L, ALT 27 U/L, total bilirubin 0.8 mg/dL, alkaline phosphatase 151 IU/L, lipase 395 IU/L. Computed Tomography (CT) abdomen showed a large 10x10 cm pancreatic head pseudocyst compressing the superior mesenteric vein, common bile duct (measured 18 mm), and stomach (seen in figure 1), and a 10x8x6 cm pseudocyst in the pancreatic tail. EUS demonstrated the pancreatic tail pseudocyst that collapsed with fluid aspiration, and a walled-off pancreatic necrosis (WOPN) in the pancreatic head with evidence of extensive intervening vasculature which made lumen-apposing metal stent (LAMS) stent placement impossible. Interventional radiology (IR) was consulted for drainage of the larger cyst, however repeat CT demonstrated interval enlargement with internal hemorrhage. On CT angiography, active intracystic bleeding was noted from a pseudoaneurysm arising from a branch of the inferior pancreaticoduodenal artery, which was successfully embolized by IR. The patient was discharged after remaining hemodynamically stable with no worsening anemia. She was readmitted two weeks later with recurrent abdominal pain and emesis. Repeat EUS showed stable 8x8 cm hemorrhagic pancreatic head pseudocyst with a clear window for successful cystgastrostomy AXIOS LAMS placement.
Discussion: Pancreatitis can result in pancreatic pseudocysts in ~ 1 per 100,000 and are frequently managed endoscopically by either fine needle aspiration or placement of a LAMS in the case of necrotic pseudocyst. In less than 10% of cases, this inflammation can also result in the development of pancreatic pseudoaneurysms, and if bleeding occurs, mortality can reach up to 40%. Thus, this case demonstrates the importance of thorough imaging and endoscopic evaluation of the pancreas and fluid cavity prior to endoscopic therapeutic management to prevent further bleeding complications.

Figure: Figure 1: CT abdomen with contrast demonstrating a large 10x10 cm pancreatic head pseudocyst causing compression of surrounding structures
Disclosures:
Ahila Manivannan indicated no relevant financial relationships.
William Davis indicated no relevant financial relationships.
Stephanie Betcher indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Ahila Manivannan, MD1, William Davis, DO2, Stephanie Betcher, MD1, Robert Pompa, MD2. P0867 - Management of a Necrotic Pancreatic Pseudocyst – Avoiding the Dreaded Pseudoaneurysm Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
