Sunday Poster Session
Category: Interventional Endoscopy
P0874 - A Unique Case of a Migrated Plastic Stents Resulting in Delayed Pancreatitis Following EDGE Procedure
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Taher Jamali, MD
Henry Ford Health
Farmington Hills, MI
Presenting Author(s)
Taher Jamali, MD1, Mazen Elatrache, MD2, Tobias Zuchelli, MD2, Sumit Singla, MD2
1Henry Ford Health, Farmington Hills, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Here we present the unique case of plastic stents originally placed within a transgastric lumen apposing metal stent (LAMS) that migrated and likely resulted in pancreatic duct (PD) stent obstruction and subsequent pancreatitis.
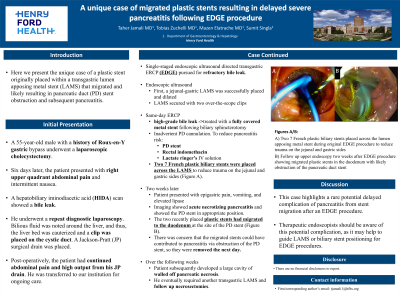
Case Description/Methods: A 55-year-old male with a history of Roux-en-Y gastric bypass underwent a laparoscopic cholecystectomy. Six days later, the patient presented with right upper quadrant abdominal pain and intermittent nausea. A hepatobiliary iminodiacetic acid (HIDA) scan showed a bile leak. He underwent a repeat diagnostic laparoscopy. Bilious fluid was noted around the liver, and thus, the liver bed was cauterized and a clip was placed on the cystic duct. A Jackson-Pratt (JP) surgical drain was placed. Post-operatively, the patient had continued abdominal pain and high output from his JP drain. He was transferred to our institution for ongoing care. Given his refractory bile leak, a single-staged endoscopic ultrasound directed transgastric ERCP (EDGE) was pursued. First, a jejunal-gastric LAMS was successfully placed, dilated, and secured with two over-the-scope clips to facilitate endoscopic biliary access through the excluded stomach. Then, during the same-day ERCP, a high-grade bile leak was treated with a fully covered metal stent following biliary sphincterotomy. A PD stent was placed due to inadvertent PD cannulation. The patient also received rectal indomethacin and lactate ringer’s intravenous solution to reduce pancreatitis risk. Two 7 French plastic biliary stents were placed across the LAMS to reduce trauma on the jejunal and gastric sides (1A). Two weeks later, the patient presented with epigastric pain, vomiting, and elevated lipase. Imaging showed acute necrotizing pancreatitis and showed the PD stent in appropriate position. The two recently placed plastic stents had migrated to the duodenum at the site of the PD stent (1B). There was concern that the migrated stents could have contributed to pancreatitis via obstruction of the PD stent, so they were removed the next day. Over the following weeks, the patient subsequently developed a large cavity of walled off pancreatic necrosis. He eventually required another transgastric LAMS and follow up necrosectomies.
Discussion: This case highlights a rare potential delayed complication of pancreatitis from stent migration after an EDGE procedure. Therapeutic endoscopists should be aware of this potential complication, as it may help to guide LAMS or biliary stent positioning for EDGE procedures.

Disclosures:
Taher Jamali, MD1, Mazen Elatrache, MD2, Tobias Zuchelli, MD2, Sumit Singla, MD2. P0874 - A Unique Case of a Migrated Plastic Stents Resulting in Delayed Pancreatitis Following EDGE Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health, Farmington Hills, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Here we present the unique case of plastic stents originally placed within a transgastric lumen apposing metal stent (LAMS) that migrated and likely resulted in pancreatic duct (PD) stent obstruction and subsequent pancreatitis.
Case Description/Methods: A 55-year-old male with a history of Roux-en-Y gastric bypass underwent a laparoscopic cholecystectomy. Six days later, the patient presented with right upper quadrant abdominal pain and intermittent nausea. A hepatobiliary iminodiacetic acid (HIDA) scan showed a bile leak. He underwent a repeat diagnostic laparoscopy. Bilious fluid was noted around the liver, and thus, the liver bed was cauterized and a clip was placed on the cystic duct. A Jackson-Pratt (JP) surgical drain was placed. Post-operatively, the patient had continued abdominal pain and high output from his JP drain. He was transferred to our institution for ongoing care. Given his refractory bile leak, a single-staged endoscopic ultrasound directed transgastric ERCP (EDGE) was pursued. First, a jejunal-gastric LAMS was successfully placed, dilated, and secured with two over-the-scope clips to facilitate endoscopic biliary access through the excluded stomach. Then, during the same-day ERCP, a high-grade bile leak was treated with a fully covered metal stent following biliary sphincterotomy. A PD stent was placed due to inadvertent PD cannulation. The patient also received rectal indomethacin and lactate ringer’s intravenous solution to reduce pancreatitis risk. Two 7 French plastic biliary stents were placed across the LAMS to reduce trauma on the jejunal and gastric sides (1A). Two weeks later, the patient presented with epigastric pain, vomiting, and elevated lipase. Imaging showed acute necrotizing pancreatitis and showed the PD stent in appropriate position. The two recently placed plastic stents had migrated to the duodenum at the site of the PD stent (1B). There was concern that the migrated stents could have contributed to pancreatitis via obstruction of the PD stent, so they were removed the next day. Over the following weeks, the patient subsequently developed a large cavity of walled off pancreatic necrosis. He eventually required another transgastric LAMS and follow up necrosectomies.
Discussion: This case highlights a rare potential delayed complication of pancreatitis from stent migration after an EDGE procedure. Therapeutic endoscopists should be aware of this potential complication, as it may help to guide LAMS or biliary stent positioning for EDGE procedures.

Figure: Figure 1: A) Two 7 French plastic biliary stents placed across the lumen apposing metal stent during original EDGE procedure to reduce trauma on the jejunal and gastric sides B) Follow up upper endoscopy two weeks after EDGE procedure showing migrated plastic stents in the duodenum with likely obstruction of the pancreatic duct stent
Disclosures:
Taher Jamali indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Sumit Singla: Boston Scientific – Consultant.
Taher Jamali, MD1, Mazen Elatrache, MD2, Tobias Zuchelli, MD2, Sumit Singla, MD2. P0874 - A Unique Case of a Migrated Plastic Stents Resulting in Delayed Pancreatitis Following EDGE Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
