Sunday Poster Session
Category: Interventional Endoscopy
P0880 - Duodeno-Colonic Fistula Stenting in the Colorectal Cancer
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- SN
Soo-Young Na, MD, PhD
Incheon St. Mary's Hospital, The Catholic University of Korea
Incheon, Inch'on-jikhalsi, Republic of Korea
Presenting Author(s)
Soo-Young Na, MD, PhD, Jeong-seon Ji, MD, PhD, Hwang Choi, MD, PhD
Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon, Inch'on-jikhalsi, Republic of Korea
Introduction: Colonic stenting is performed as a bridge to surgery or palliative in malignant colorectal obstruction. Complications such as tumor overgrowth or ingrowth, stent migration, and perforation could occur. Here, we report a rare case of entero-colonic stenting due to a duodeno-colonic fistula of colorectal cancer.
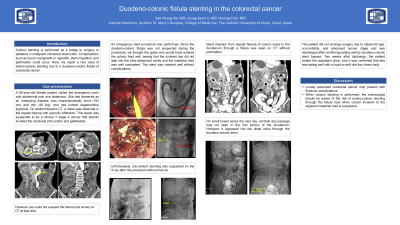
Case Description/Methods: A 90-year-old female patient visited the emergency room with abdominal pain and distension. She had dementia as an underlying disease, was characteristically short (150 cm) and thin (40 Kg), and had lumbar degenerative kyphosis. On abdominopelvic CT, a mass was observed in the hepatic flexure with pericolic infiltration. This lesion was suspected to be a clinical T stage 4 cancer that directly invaded the duodenal 2nd portion and gallbladder (Fig. 1A). An emergency stent procedure was performed. Since the duodeno-colonic fistula was not suspected during the procedure, we thought the guide wire would have entered the colonic tract well, seeing that the contrast dye did not leak into the intra-abdominal cavity and the intestinal tract was well contrasted. The stent was inserted well without complications. However, unfortunately, entero-colonic stenting was suspected on the plain X-ray after the procedure without free air (Fig. 1B). Stent insertion from hepatic flexure of the colonic mass to the duodenum through a fistula was seen on CT without perforation (Fig. 1C). On small bowel series the next day, contrast dye passage was not seen in the 2nd portion of the duodenum. However, it bypassed into the distal colon through the duodeno-colonic stent (Fig. 1D). The patient did not undergo surgery due to oldest-old age, co-morbidity, and advanced cancer stage and was discharged after confirming eating well by duodeno-colonic stent bypass. Two weeks after discharge, the patient visited the outpatient clinic, and it was confirmed that she was eating well with a liquid-to-soft diet four times daily.
Discussion: Locally advanced colorectal cancer may present with fistulous complications. When colonic stenting is performed, the endoscopist should be aware of the risk of entero-colonic stenting through the fistula tract when cancer invasion to the adjacent intestinal tract is suspected.

Disclosures:
Soo-Young Na, MD, PhD, Jeong-seon Ji, MD, PhD, Hwang Choi, MD, PhD. P0880 - Duodeno-Colonic Fistula Stenting in the Colorectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon, Inch'on-jikhalsi, Republic of Korea
Introduction: Colonic stenting is performed as a bridge to surgery or palliative in malignant colorectal obstruction. Complications such as tumor overgrowth or ingrowth, stent migration, and perforation could occur. Here, we report a rare case of entero-colonic stenting due to a duodeno-colonic fistula of colorectal cancer.
Case Description/Methods: A 90-year-old female patient visited the emergency room with abdominal pain and distension. She had dementia as an underlying disease, was characteristically short (150 cm) and thin (40 Kg), and had lumbar degenerative kyphosis. On abdominopelvic CT, a mass was observed in the hepatic flexure with pericolic infiltration. This lesion was suspected to be a clinical T stage 4 cancer that directly invaded the duodenal 2nd portion and gallbladder (Fig. 1A). An emergency stent procedure was performed. Since the duodeno-colonic fistula was not suspected during the procedure, we thought the guide wire would have entered the colonic tract well, seeing that the contrast dye did not leak into the intra-abdominal cavity and the intestinal tract was well contrasted. The stent was inserted well without complications. However, unfortunately, entero-colonic stenting was suspected on the plain X-ray after the procedure without free air (Fig. 1B). Stent insertion from hepatic flexure of the colonic mass to the duodenum through a fistula was seen on CT without perforation (Fig. 1C). On small bowel series the next day, contrast dye passage was not seen in the 2nd portion of the duodenum. However, it bypassed into the distal colon through the duodeno-colonic stent (Fig. 1D). The patient did not undergo surgery due to oldest-old age, co-morbidity, and advanced cancer stage and was discharged after confirming eating well by duodeno-colonic stent bypass. Two weeks after discharge, the patient visited the outpatient clinic, and it was confirmed that she was eating well with a liquid-to-soft diet four times daily.
Discussion: Locally advanced colorectal cancer may present with fistulous complications. When colonic stenting is performed, the endoscopist should be aware of the risk of entero-colonic stenting through the fistula tract when cancer invasion to the adjacent intestinal tract is suspected.

Figure: Fig. 1. A, Initial abdomino-pelvic CT. B, Plain X-ray immediately after stent insertion. C, Abdomino-pelvic CT on the day after stent insertion. D, Small bowel series the next day after stent insertion.
Disclosures:
Soo-Young Na indicated no relevant financial relationships.
Jeong-seon Ji indicated no relevant financial relationships.
Hwang Choi indicated no relevant financial relationships.
Soo-Young Na, MD, PhD, Jeong-seon Ji, MD, PhD, Hwang Choi, MD, PhD. P0880 - Duodeno-Colonic Fistula Stenting in the Colorectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
