Sunday Poster Session
Category: Interventional Endoscopy
P0881 - Endoscopic Management of Pancreatic Ascites Following Surgical Fenestration of a Large Symptomatic Hepatic Cyst
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Kristen Fadel, MD
New York-Presbyterian Hospital/Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Kristen Fadel, MD1, Lasha Gogokhia, MD1, Johannes Untch, 2, Sanjay Salgado, MD1, Kartik Sampath, MD1
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2Technische Universität München, School of Medicine, München, Bayern, Germany
Introduction: Pancreatic duct (PD) leak is an uncommon complication of acute pancreatitis, trauma, and/or iatrogenic post-surgical injury. High grade leaks can lead to refractory symptomatic pancreatic ascites. Management can include observation, percutaneous catheter drainage, surgical revision, endoscopic retrograde cholangiopancreatography (ERCP) and/or endoscopic ultrasound (EUS) guided drainage. Herein we report the successful endoscopic management of pancreatic leak/ascites following surgical hepatic cyst fenestration.
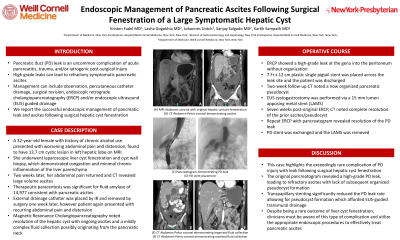
Case Description/Methods: A 32-year-old female with history of chronic alcohol use presented with worsening abdominal pain and distension, found to have a 13.7 cm cystic lesion in the left hepatic lobe on MRI. She underwent laparoscopic liver cyst fenestration and cyst wall biopsy, which demonstrated congestion and minimal chronic inflammation of the liver parenchyma. Two weeks later, her abdominal pain returned and CT revealed large volume ascites. Therapeutic paracentesis was significant for a fluid amylase of 14,977 consistent with pancreatic ascites, and percutaneous drain was placed. Magnetic Resonance Cholangiopancreatography noted resolution of the hepatic cyst with ongoing ascites and a mildly complex fluid collection possibly originating from the pancreatic neck. ERCP showed a high-grade leak at the genu into the peritoneum without organization. A 7 Fr x 12 cm plastic single pigtail stent was placed across the leak site and the patient was discharged. Two-week follow-up CT noted a now organized pancreatic pseudocyst and EUS cystogastrostomy was performed via a 15 mm lumen apposing metal stent (LAMS). Seven weeks post-original ERCP, the external drain was removed and CT noted complete resolution of the prior ascites/pseudocyst. Repeat ERCP with pancreatogram revealed resolution of the PD leak. The PD stent was exchanged and the LAMS was removed.
Discussion: This case highlights the exceedingly rare complication of PD injury with leak following surgical hepatic cyst fenestration. The original pancreatogram revealed a high-grade PD leak which led to refractory ascites with lack of subsequent organized pseudocyst formation. Transpapillary stenting significantly reduced the PD leak rate allowing for pseudocyst formation which afforded EUS-guided transmural drainage. Despite being a rare outcome of liver cyst fenestration, clinicians must be aware of this type of complication and utilize the appropriate endoscopic procedures to effectively treat pancreatic ascites.

Disclosures:
Kristen Fadel, MD1, Lasha Gogokhia, MD1, Johannes Untch, 2, Sanjay Salgado, MD1, Kartik Sampath, MD1. P0881 - Endoscopic Management of Pancreatic Ascites Following Surgical Fenestration of a Large Symptomatic Hepatic Cyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2Technische Universität München, School of Medicine, München, Bayern, Germany
Introduction: Pancreatic duct (PD) leak is an uncommon complication of acute pancreatitis, trauma, and/or iatrogenic post-surgical injury. High grade leaks can lead to refractory symptomatic pancreatic ascites. Management can include observation, percutaneous catheter drainage, surgical revision, endoscopic retrograde cholangiopancreatography (ERCP) and/or endoscopic ultrasound (EUS) guided drainage. Herein we report the successful endoscopic management of pancreatic leak/ascites following surgical hepatic cyst fenestration.
Case Description/Methods: A 32-year-old female with history of chronic alcohol use presented with worsening abdominal pain and distension, found to have a 13.7 cm cystic lesion in the left hepatic lobe on MRI. She underwent laparoscopic liver cyst fenestration and cyst wall biopsy, which demonstrated congestion and minimal chronic inflammation of the liver parenchyma. Two weeks later, her abdominal pain returned and CT revealed large volume ascites. Therapeutic paracentesis was significant for a fluid amylase of 14,977 consistent with pancreatic ascites, and percutaneous drain was placed. Magnetic Resonance Cholangiopancreatography noted resolution of the hepatic cyst with ongoing ascites and a mildly complex fluid collection possibly originating from the pancreatic neck. ERCP showed a high-grade leak at the genu into the peritoneum without organization. A 7 Fr x 12 cm plastic single pigtail stent was placed across the leak site and the patient was discharged. Two-week follow-up CT noted a now organized pancreatic pseudocyst and EUS cystogastrostomy was performed via a 15 mm lumen apposing metal stent (LAMS). Seven weeks post-original ERCP, the external drain was removed and CT noted complete resolution of the prior ascites/pseudocyst. Repeat ERCP with pancreatogram revealed resolution of the PD leak. The PD stent was exchanged and the LAMS was removed.
Discussion: This case highlights the exceedingly rare complication of PD injury with leak following surgical hepatic cyst fenestration. The original pancreatogram revealed a high-grade PD leak which led to refractory ascites with lack of subsequent organized pseudocyst formation. Transpapillary stenting significantly reduced the PD leak rate allowing for pseudocyst formation which afforded EUS-guided transmural drainage. Despite being a rare outcome of liver cyst fenestration, clinicians must be aware of this type of complication and utilize the appropriate endoscopic procedures to effectively treat pancreatic ascites.

Figure: (A) MRI abdomen coronal with original hepatic cyst pre-fenestration. (B) CT Abdomen Pelvis coronal demonstrating ascites. (C) Pancreatogram demonstrating PD leak. (D) PD stent placement. (E) CT abdomen pelvis coronal demonstrating organized fluid collection. (F) CT abdomen pelvis coronal demonstrating resolved fluid collection.
Disclosures:
Kristen Fadel indicated no relevant financial relationships.
Lasha Gogokhia indicated no relevant financial relationships.
Johannes Untch indicated no relevant financial relationships.
Sanjay Salgado indicated no relevant financial relationships.
Kartik Sampath indicated no relevant financial relationships.
Kristen Fadel, MD1, Lasha Gogokhia, MD1, Johannes Untch, 2, Sanjay Salgado, MD1, Kartik Sampath, MD1. P0881 - Endoscopic Management of Pancreatic Ascites Following Surgical Fenestration of a Large Symptomatic Hepatic Cyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
