Sunday Poster Session
Category: Interventional Endoscopy
P0884 - Achalasia or Pseudoachalasia: Incidental Esophagogastric Junction Submucosal Leiomyoma During Peroral Endoscopic Myotomy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- CC
Cynthia Contreras, MD
TriHealth
Cincinnati, Ohio
Presenting Author(s)
M Kenan Rahima, MD, Venkata Muddana, MD, Mohamad Hijazi, MD, Cynthia Contreras, MD, Usha Thapa, MD, Amin Eshghabadi, MD
TriHealth, Cincinnati, OH
Introduction: The concomitant presence of achalasia and esophagogastric junction (EGJ) leiomyoma is extremely rare. To the best of our knowledge, there are no reported cases of esophageal achalasia and EGJ leiomyoma co-existence. We present a case where clinical assessment, endoscopic, manometric and radiological evaluation revealed the diagnosis of type II achalasia. Eventually, the patient underwent peroral endoscopic myotomy (POEM) which revealed an incidental leiomyoma that was found at EGJ which was removed with submucosal tunnelling endoscopic resection (STER).
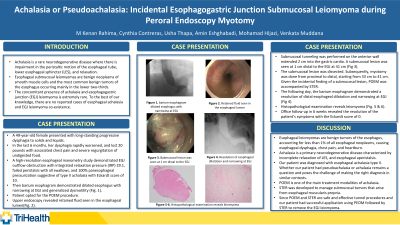
Case Description/Methods: A 49-year-old female presented with long standing progressive dysphagia to solids and liquids. A high-resolution esophageal manometry study demonstrated EGJ outflow obstruction, failed peristalsis with all swallows and 100% panesophageal pressurization suggestive of type II achalasia with Eckardt score of 10. Then barium esophagram demonstrated dilated esophagus with narrowing at EGJ and generalized dysmotility (Fig.1). Patient opted for POEM procedure. Endoluminal functional lumen imaging probe (EndoFLIP) measurements before myotomy reveals low EGJ distensibility index. Subsequently, upper endoscopy revealed EGJ at ~40 cm, retained fluid seen in the esophageal lumen and no other abnormalities (Fig.2). Submucosal tunnelling and submucosal lesion was seen at EGJ which was dissected from the submucosa and muscularis propria (Fig.3). Subsequently, myotomy was done from proximal to distal starting from 33 cm to 41 cm. Given the incidental finding of a submucosal lesion, POEM was accompanied with STER. EndoFLIP measurements post myotomy reveal normalization of EGJ distensibility index. Barium esophagram demonstrated a resolution of distal esophageal dilatation and narrowing of the EGJ (Fig.4). Histopathological examination reveals leiomyoma (Fig.5&6). Office follow up in 6 weeks reveal symptoms have resolved with Eckardt score of 0.
Discussion: Achalasia and pseudoachalasia can have similar clinical presentation, radiological assessment, and endoscopic findings. Therefore, a high index of suspicion of pseudoachalasia should be maintained. An additional measure we could’ve performed is EUS, thus this case presentation supports the use of EUS as a final measure to rule out possible submucosal tumors. Whether our patient had pseudoachalasia or achalasia remains a question.
The patient had PEOM followed by STER to remove the EGJ leiomyoma with optimal results suggesting that STER is a viable option to manage EGJ leiomyoma.

Disclosures:
M Kenan Rahima, MD, Venkata Muddana, MD, Mohamad Hijazi, MD, Cynthia Contreras, MD, Usha Thapa, MD, Amin Eshghabadi, MD. P0884 - Achalasia or Pseudoachalasia: Incidental Esophagogastric Junction Submucosal Leiomyoma During Peroral Endoscopic Myotomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
TriHealth, Cincinnati, OH
Introduction: The concomitant presence of achalasia and esophagogastric junction (EGJ) leiomyoma is extremely rare. To the best of our knowledge, there are no reported cases of esophageal achalasia and EGJ leiomyoma co-existence. We present a case where clinical assessment, endoscopic, manometric and radiological evaluation revealed the diagnosis of type II achalasia. Eventually, the patient underwent peroral endoscopic myotomy (POEM) which revealed an incidental leiomyoma that was found at EGJ which was removed with submucosal tunnelling endoscopic resection (STER).
Case Description/Methods: A 49-year-old female presented with long standing progressive dysphagia to solids and liquids. A high-resolution esophageal manometry study demonstrated EGJ outflow obstruction, failed peristalsis with all swallows and 100% panesophageal pressurization suggestive of type II achalasia with Eckardt score of 10. Then barium esophagram demonstrated dilated esophagus with narrowing at EGJ and generalized dysmotility (Fig.1). Patient opted for POEM procedure. Endoluminal functional lumen imaging probe (EndoFLIP) measurements before myotomy reveals low EGJ distensibility index. Subsequently, upper endoscopy revealed EGJ at ~40 cm, retained fluid seen in the esophageal lumen and no other abnormalities (Fig.2). Submucosal tunnelling and submucosal lesion was seen at EGJ which was dissected from the submucosa and muscularis propria (Fig.3). Subsequently, myotomy was done from proximal to distal starting from 33 cm to 41 cm. Given the incidental finding of a submucosal lesion, POEM was accompanied with STER. EndoFLIP measurements post myotomy reveal normalization of EGJ distensibility index. Barium esophagram demonstrated a resolution of distal esophageal dilatation and narrowing of the EGJ (Fig.4). Histopathological examination reveals leiomyoma (Fig.5&6). Office follow up in 6 weeks reveal symptoms have resolved with Eckardt score of 0.
Discussion: Achalasia and pseudoachalasia can have similar clinical presentation, radiological assessment, and endoscopic findings. Therefore, a high index of suspicion of pseudoachalasia should be maintained. An additional measure we could’ve performed is EUS, thus this case presentation supports the use of EUS as a final measure to rule out possible submucosal tumors. Whether our patient had pseudoachalasia or achalasia remains a question.
The patient had PEOM followed by STER to remove the EGJ leiomyoma with optimal results suggesting that STER is a viable option to manage EGJ leiomyoma.

Figure: Leiomyoma Images
Disclosures:
M Kenan Rahima indicated no relevant financial relationships.
Venkata Muddana indicated no relevant financial relationships.
Mohamad Hijazi indicated no relevant financial relationships.
Cynthia Contreras indicated no relevant financial relationships.
Usha Thapa indicated no relevant financial relationships.
Amin Eshghabadi indicated no relevant financial relationships.
M Kenan Rahima, MD, Venkata Muddana, MD, Mohamad Hijazi, MD, Cynthia Contreras, MD, Usha Thapa, MD, Amin Eshghabadi, MD. P0884 - Achalasia or Pseudoachalasia: Incidental Esophagogastric Junction Submucosal Leiomyoma During Peroral Endoscopic Myotomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
