Sunday Poster Session
Category: Interventional Endoscopy
P0887 - Endoscopic Underwater Ampullectomy Technique for a Sporadic Ampullary Adenoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Asad Rehman, DO
HCA Healthcare
Houston, TX
Presenting Author(s)
Asad Rehman, DO1, Bobby Jacob, MD2, Meir Mizrahi, MD3
1HCA Healthcare, Largo, FL; 2HCA Florida Largo Hospital, Largo, FL; 3Largo Medical Center, Largo, FL
Introduction: Endoscopic ampullectomy (EA) is a high-risk procedure due to the complex nature of the ampulla, which connects the duodenum, bile duct, and pancreatic duct. EA is increasingly being used and has lower mortality rates compared to surgical approaches. Our study aims to add to the literature on the efficacy of EA in preventing malignant transformation and to demonstrate the use of underwater EA technique for a large ampullary adenoma (AA).
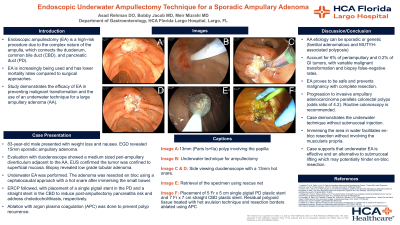
Case Description/Methods: An 83-year-old male underwent endoscopic evaluation for weight loss and nausea, revealing a large 15mm sporadic ampullary adenoma. Colonoscopy ruled out colonic neoplasia. The patient was referred for endoscopic resection. Evaluation with a side-viewing duodenoscope showed a medium sized peri-ampullary diverticulum adjacent to the ampullary adenoma. EUS confirmed the tumor was confined to superficial mucosal. Biopsy supported the decision for EA, as it revealed low grade tubular adenoma. Underwater EA was performed using a side-viewing duodenoscope. The adenoma was resected en bloc using a cephalocaudal approach with a 13mm hot snare after immersing the small bowel. ERCP followed, with placement of both a 5Frx5cm single pigtail and 7Frx7cm stent in the common bile duct to reduce post-ampullectomy pancreatitis risk and address choledocholithiasis, respectively. Ablation with argon plasma coagulation was done to prevent polyp recurrence. Pathology confirmed low-grade tubular adenoma. Repeat surveillance endoscopy was scheduled within six months.
Discussion: AAs can be sporadic or associated with genetic conditions such as familial adenomatous and MUTYH-associated polyposis. AAs account for only 6% of periampullary and 0.2% of gastrointestinal tumors, with variable malignant transformation rates and biopsy false-negative rates. EA by experienced endoscopists is safe and prevents malignancy with complete resection. Progression to invasive ampullary adenocarcinoma parallels colorectal polyps with early mutations in ABCB1 and has an odds ratio of 4.2, hence why routine colonoscopy is recommended. Various EA techniques exist. In this study, the underwater technique without submucosal injection was used. Immersing the area in water facilitates en-bloc resection without involving the muscularis propria. There is no established standard approach for EA, however our case supports that underwater endoscopic ampullectomy is effective and an alternative to submucosal lifting which may potentially hinder en-bloc resection.

Disclosures:
Asad Rehman, DO1, Bobby Jacob, MD2, Meir Mizrahi, MD3. P0887 - Endoscopic Underwater Ampullectomy Technique for a Sporadic Ampullary Adenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Healthcare, Largo, FL; 2HCA Florida Largo Hospital, Largo, FL; 3Largo Medical Center, Largo, FL
Introduction: Endoscopic ampullectomy (EA) is a high-risk procedure due to the complex nature of the ampulla, which connects the duodenum, bile duct, and pancreatic duct. EA is increasingly being used and has lower mortality rates compared to surgical approaches. Our study aims to add to the literature on the efficacy of EA in preventing malignant transformation and to demonstrate the use of underwater EA technique for a large ampullary adenoma (AA).
Case Description/Methods: An 83-year-old male underwent endoscopic evaluation for weight loss and nausea, revealing a large 15mm sporadic ampullary adenoma. Colonoscopy ruled out colonic neoplasia. The patient was referred for endoscopic resection. Evaluation with a side-viewing duodenoscope showed a medium sized peri-ampullary diverticulum adjacent to the ampullary adenoma. EUS confirmed the tumor was confined to superficial mucosal. Biopsy supported the decision for EA, as it revealed low grade tubular adenoma. Underwater EA was performed using a side-viewing duodenoscope. The adenoma was resected en bloc using a cephalocaudal approach with a 13mm hot snare after immersing the small bowel. ERCP followed, with placement of both a 5Frx5cm single pigtail and 7Frx7cm stent in the common bile duct to reduce post-ampullectomy pancreatitis risk and address choledocholithiasis, respectively. Ablation with argon plasma coagulation was done to prevent polyp recurrence. Pathology confirmed low-grade tubular adenoma. Repeat surveillance endoscopy was scheduled within six months.
Discussion: AAs can be sporadic or associated with genetic conditions such as familial adenomatous and MUTYH-associated polyposis. AAs account for only 6% of periampullary and 0.2% of gastrointestinal tumors, with variable malignant transformation rates and biopsy false-negative rates. EA by experienced endoscopists is safe and prevents malignancy with complete resection. Progression to invasive ampullary adenocarcinoma parallels colorectal polyps with early mutations in ABCB1 and has an odds ratio of 4.2, hence why routine colonoscopy is recommended. Various EA techniques exist. In this study, the underwater technique without submucosal injection was used. Immersing the area in water facilitates en-bloc resection without involving the muscularis propria. There is no established standard approach for EA, however our case supports that underwater endoscopic ampullectomy is effective and an alternative to submucosal lifting which may potentially hinder en-bloc resection.

Figure: Image A) 13mm (Paris Is+IIa) polyp involving the papilla. Image B) Underwater technique for ampullectomy. Images C & D) Side viewing duodenoscope with a 13mm hot snare. Image E) Retrieval of the specimen using rescue net. Image F) Placement of 5 Fr x 5 cm single pigtail pancreatic duct plastic stent and 7 Fr x 7 cm straight common bile duct plastic stent. Residual polypoid tissue treated with hot avulsion technique and resection borders ablated using argon plasma coagulation (APC).
Disclosures:
Asad Rehman indicated no relevant financial relationships.
Bobby Jacob indicated no relevant financial relationships.
Meir Mizrahi: Boston Scientific – Consultant. COOK medical – Consultant. Fujifilm – Consultant. Medtronic – Consultant.
Asad Rehman, DO1, Bobby Jacob, MD2, Meir Mizrahi, MD3. P0887 - Endoscopic Underwater Ampullectomy Technique for a Sporadic Ampullary Adenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
