Sunday Poster Session
Category: Interventional Endoscopy
P0902 - Isolated Duodenal Varices: A Rare Presentation of Occult Bleeding Managed With Endoscopic Sclerotherapy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AS
Ashley Scholtens, MD
Creighton University
Phoenix, AZ
Presenting Author(s)
Ashley Scholtens, MD1, Brett Hughes, MD2, Neil Vyas, MD1, Subhash Chandra, MD2, Savio Reddymasu, MD1
1Creighton University, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ
Introduction: Duodenal varices (DV) are a rare manifestation of portal HTN associated with significant GI bleeding, management difficulties, and high mortality rates. We present a case of endoscopically diagnosed isolated DV’s presenting as occult bleeding, successfully managed using sclerotherapy via esophagogastroduodenoscopy (EGD).
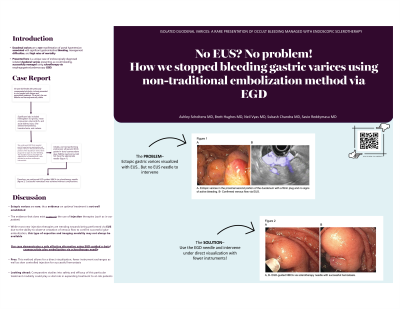
Case Description/Methods: A 35-year-old female with previously compensated alcoholic cirrhosis presented with fatigue and weakness. On arrival, she was afebrile and hemodynamically stable. Significant labs included Hgb 5.0 gm/dL, MCV 86 fL, and AKI. She denied hematemesis, hematochezia, or melena. She was transfused packed RBC with an inappropriate response in Hgb, thus underwent EGD that revealed portal hypertensive gastropathy and ectopic varices in the proximal second portion of the duodenum with a fibrin plug and no signs of active bleeding. The DV’s had high-risk stigmata for re-bleeding thus it was decided to perform endoscopic intervention. Initially, we tried performing endoscopic ultrasound (EUS) guided n-butyl cyanoacrylate glue (NBCA) injection but did not have the appropriate needle (figure 1). Therefore, we performed EGD-guided NBCA via sclerotherapy needle (figure 2). Successful hemostasis was achieved without complications.
Discussion: It is important to maintain a high index of suspicion in all patients with cirrhosis presenting with occult GI bleeding given the wide list of potential etiologies. As seen in our patient, prompt endoscopic evaluation may allow for endoscopic management otherwise not available if left undiagnosed given the potential for rapid decompensation. Optimal treatment of ectopic varices is not well established given their rare occurrence. New evidence from a recent systematic review concluded that injection therapies such as in our patient may be preferable in the management of duodenal variceal bleeding. New injection therapies are trending towards being performed via EUS due to the ability to observe cessation of venous flow to confirm successful glue embolization, however, this type of expertise and imaging modality may not always be available. Our case demonstrates a safe, effective alternative using EGD-guided NBCA glue embolization via sclerotherapy needle. This method allows for direct visualization, fewer instrument exchanges, and slow controlled injection for successful hemostasis. Comparative studies into safety and efficacy of this particular treatment modality could play a vital role in expanding treatment to at-risk patients.

Disclosures:
Ashley Scholtens, MD1, Brett Hughes, MD2, Neil Vyas, MD1, Subhash Chandra, MD2, Savio Reddymasu, MD1. P0902 - Isolated Duodenal Varices: A Rare Presentation of Occult Bleeding Managed With Endoscopic Sclerotherapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ
Introduction: Duodenal varices (DV) are a rare manifestation of portal HTN associated with significant GI bleeding, management difficulties, and high mortality rates. We present a case of endoscopically diagnosed isolated DV’s presenting as occult bleeding, successfully managed using sclerotherapy via esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 35-year-old female with previously compensated alcoholic cirrhosis presented with fatigue and weakness. On arrival, she was afebrile and hemodynamically stable. Significant labs included Hgb 5.0 gm/dL, MCV 86 fL, and AKI. She denied hematemesis, hematochezia, or melena. She was transfused packed RBC with an inappropriate response in Hgb, thus underwent EGD that revealed portal hypertensive gastropathy and ectopic varices in the proximal second portion of the duodenum with a fibrin plug and no signs of active bleeding. The DV’s had high-risk stigmata for re-bleeding thus it was decided to perform endoscopic intervention. Initially, we tried performing endoscopic ultrasound (EUS) guided n-butyl cyanoacrylate glue (NBCA) injection but did not have the appropriate needle (figure 1). Therefore, we performed EGD-guided NBCA via sclerotherapy needle (figure 2). Successful hemostasis was achieved without complications.
Discussion: It is important to maintain a high index of suspicion in all patients with cirrhosis presenting with occult GI bleeding given the wide list of potential etiologies. As seen in our patient, prompt endoscopic evaluation may allow for endoscopic management otherwise not available if left undiagnosed given the potential for rapid decompensation. Optimal treatment of ectopic varices is not well established given their rare occurrence. New evidence from a recent systematic review concluded that injection therapies such as in our patient may be preferable in the management of duodenal variceal bleeding. New injection therapies are trending towards being performed via EUS due to the ability to observe cessation of venous flow to confirm successful glue embolization, however, this type of expertise and imaging modality may not always be available. Our case demonstrates a safe, effective alternative using EGD-guided NBCA glue embolization via sclerotherapy needle. This method allows for direct visualization, fewer instrument exchanges, and slow controlled injection for successful hemostasis. Comparative studies into safety and efficacy of this particular treatment modality could play a vital role in expanding treatment to at-risk patients.

Figure: Figure 1: A- Ectopic varices in the proximal second portion of the duodenum with a fibrin plug and no signs of active bleeding. B-Confirmed venous flow via EUS.
Figure 2: A,B- EGD-guided NBCA via sclerotherapy needle with successful hemostasis.
Figure 2: A,B- EGD-guided NBCA via sclerotherapy needle with successful hemostasis.
Disclosures:
Ashley Scholtens indicated no relevant financial relationships.
Brett Hughes indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Subhash Chandra indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Ashley Scholtens, MD1, Brett Hughes, MD2, Neil Vyas, MD1, Subhash Chandra, MD2, Savio Reddymasu, MD1. P0902 - Isolated Duodenal Varices: A Rare Presentation of Occult Bleeding Managed With Endoscopic Sclerotherapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
