Sunday Poster Session
Category: Interventional Endoscopy
P0903 - EDGE Gone Wrong! Salvaged Using a NOTES-Style Technique
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DC
David L. Cheung, MD
UC Irvine
Orange, CA
Presenting Author(s)
Award: Presidential Poster Award
David L. Cheung, MD1, Amirali Tavangar, MD2, Anastasia Chahine, MD2, Peter Nguyen, MD2, Khaldoon Khirfan, MD2, Joshua Kwon, MD2, John Lee, MD2, Jason Samarasena, MD2
1UC Irvine, Orange, CA; 2University of California Irvine, Orange, CA
Introduction: While bariatric surgery is an effective and increasingly utilized procedure to combat obesity, rapid weight loss associated with these procedures has predisposed patients to developing cholelithiasis. In the case of a Roux-En-Y Gastric bypass (RYGB), access to the native stomach and common bile duct (CBD) is endoscopically restricted. The Endoscopic ultrasound-directed transgastric ERCP (EDGE) procedure utilizes a lumen apposing metal stent (LAMS) to offer access to the gastric body and duodenum, however, stent mispositioning and perforation are associated risks of the procedure. This case demonstrates an EDGE salvage technique when the distal lumen of the LAMS has been dislodged into the peritoneal cavity.
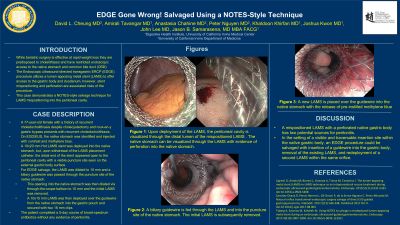
Case Description/Methods: A 77-year-old female with a history of cholecystectomy and gastric bypass presents with recurrent choledocholithiasis. She had previously undergone two laparoscopic assisted ERCPs but elected to undergo EDGE procedure for CBD evaluation. On EGD/EUS, the native stomach was identified and injected with contrast and methylene blue. A 10x20 mm Hot LAMS stent was deployed into the native stomach, but, upon withdrawal of the LAMS placement catheter, the distal end of the stent appeared open to the peritoneal cavity with a visible puncture site seen on the external gastric body surface (Image A/B). For EDGE salvage, the LAMS was dilated to 10 mm and a biliary guidewire was passed through the puncture site of the native stomach. This opening into the native stomach was then dilated via through-the-scope balloon to 10 mm and the initial LAMS was removed. A 10x15 mm LAMS was then deployed over the guidewire from the native stomach into the gastric pouch and secured with two 16 mm clips (Image C/D). The patient completed a 5-day course of broad-spectrum antibiotics without any evidence of peritonitis.
Discussion: Troubleshooting advanced endoscopic procedures can prove to be challenging. Various salvage techniques for LAMS have been documented, including use of Natural Orifice Transluminal Endoscopic Surgery (NOTES) procedure and LAMS-in-LAMS technique for re-stent placement. In this case, the mispositioned LAMS perforated the native gastric body, creating two potential sources for peritonitis. In the setting of a visible and traversable insertion site within the native gastric body, an EDGE procedure could be salvaged with insertion of a guidewire into the gastric body, removal of the existing LAMS, and redeployment of a second LAMS within the same orifice.

Disclosures:
David L. Cheung, MD1, Amirali Tavangar, MD2, Anastasia Chahine, MD2, Peter Nguyen, MD2, Khaldoon Khirfan, MD2, Joshua Kwon, MD2, John Lee, MD2, Jason Samarasena, MD2. P0903 - EDGE Gone Wrong! Salvaged Using a NOTES-Style Technique, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
David L. Cheung, MD1, Amirali Tavangar, MD2, Anastasia Chahine, MD2, Peter Nguyen, MD2, Khaldoon Khirfan, MD2, Joshua Kwon, MD2, John Lee, MD2, Jason Samarasena, MD2
1UC Irvine, Orange, CA; 2University of California Irvine, Orange, CA
Introduction: While bariatric surgery is an effective and increasingly utilized procedure to combat obesity, rapid weight loss associated with these procedures has predisposed patients to developing cholelithiasis. In the case of a Roux-En-Y Gastric bypass (RYGB), access to the native stomach and common bile duct (CBD) is endoscopically restricted. The Endoscopic ultrasound-directed transgastric ERCP (EDGE) procedure utilizes a lumen apposing metal stent (LAMS) to offer access to the gastric body and duodenum, however, stent mispositioning and perforation are associated risks of the procedure. This case demonstrates an EDGE salvage technique when the distal lumen of the LAMS has been dislodged into the peritoneal cavity.
Case Description/Methods: A 77-year-old female with a history of cholecystectomy and gastric bypass presents with recurrent choledocholithiasis. She had previously undergone two laparoscopic assisted ERCPs but elected to undergo EDGE procedure for CBD evaluation. On EGD/EUS, the native stomach was identified and injected with contrast and methylene blue. A 10x20 mm Hot LAMS stent was deployed into the native stomach, but, upon withdrawal of the LAMS placement catheter, the distal end of the stent appeared open to the peritoneal cavity with a visible puncture site seen on the external gastric body surface (Image A/B). For EDGE salvage, the LAMS was dilated to 10 mm and a biliary guidewire was passed through the puncture site of the native stomach. This opening into the native stomach was then dilated via through-the-scope balloon to 10 mm and the initial LAMS was removed. A 10x15 mm LAMS was then deployed over the guidewire from the native stomach into the gastric pouch and secured with two 16 mm clips (Image C/D). The patient completed a 5-day course of broad-spectrum antibiotics without any evidence of peritonitis.
Discussion: Troubleshooting advanced endoscopic procedures can prove to be challenging. Various salvage techniques for LAMS have been documented, including use of Natural Orifice Transluminal Endoscopic Surgery (NOTES) procedure and LAMS-in-LAMS technique for re-stent placement. In this case, the mispositioned LAMS perforated the native gastric body, creating two potential sources for peritonitis. In the setting of a visible and traversable insertion site within the native gastric body, an EDGE procedure could be salvaged with insertion of a guidewire into the gastric body, removal of the existing LAMS, and redeployment of a second LAMS within the same orifice.

Figure: A) Peritoneal cavity visualized through the distal lumen of the mispositioned LAMS
B) Native stomach visualized through the mispositioned AXIOS stent with evidence of perforation after stent deployment
C) Biliary guidewire placed through perforated native stomach
D) Placement of new LAMS into the native stomach with the release of instilled methylene blue solution
B) Native stomach visualized through the mispositioned AXIOS stent with evidence of perforation after stent deployment
C) Biliary guidewire placed through perforated native stomach
D) Placement of new LAMS into the native stomach with the release of instilled methylene blue solution
Disclosures:
David Cheung indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Anastasia Chahine indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Joshua Kwon indicated no relevant financial relationships.
John Lee indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Advisor or Review Panel Member. Boston Scientific – Consultant. Conmed – Consultant. Cook – Educational Grant. Neptune Medical – Consultant. Olympus – Consultant. Steris – Consultant.
David L. Cheung, MD1, Amirali Tavangar, MD2, Anastasia Chahine, MD2, Peter Nguyen, MD2, Khaldoon Khirfan, MD2, Joshua Kwon, MD2, John Lee, MD2, Jason Samarasena, MD2. P0903 - EDGE Gone Wrong! Salvaged Using a NOTES-Style Technique, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

