Sunday Poster Session
Category: Liver
P0918 - Association of Non-Alcoholic Fatty Liver Disease With Gastrointestinal Infections: Insights From National Inpatient Sample
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JP
Jay Patel, MD
Orange Park Medical Center
Cleveland, OH
Presenting Author(s)
Jay Patel, MD1, Aalam Sohal, MD2, Kanwal Bains, MBBS, CNSC3, Hunza Chaudhry, MD4, Isha Kohli, MBBS, CPH, MPH5, Kirti Arora, MBBS6, Shivam Kalra, MBBS7, Dino Dukovic, BS8, Marina Roytman, MD9
1Orange Park Medical Center, Jacksonville, FL; 2Liver Institute Northwest, Seattle, WA; 3University of Arizona, Tucson, AZ; 4University of California San Francisco, Fresno, CA; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 7Trident Medical Center, Charleston, SC; 8Ross University School of Medicine, Maramar, FL; 9UCSF Fresno, Fresno, CA
Introduction: Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the world. NAFLD is associated with changes in the gut microbiota and has an interplay with the body’s immune response. These changes may contribute to increased risk of infections. The current study was aimed at assessing the relationship between the presence of NAFLD and the risk of bacterial gastrointestinal(GI) infections.
Methods: We queried the National Inpatient Sample (NIS) database in 2020 and stratified the patients based on presence of NAFLD. Information was collected regarding patient demographics, hospital characteristics, Charlson comorbidity Index, coexisting comorbidities(GERD,HLD, smoking, diabetes, hypertension, obesity, OSA, IBD), as well as bacterial gastrointestinal infections. Multivariate analysis was used to identify association between NAFLD and bacterial GI infections, after adjusting for confounding factors.
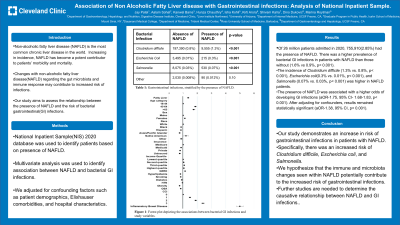
Results: A total of 26 million patients were admitted in 2020. Of these, 755,910 (2.85%) patients had the presence of NAFLD. The majority of the patients in the NAFLD group were over 65 years of age (46.1%), female (54.2%), had medicare (51.4%), and were in the lowest income quartile(30.9%)(Table 1). There was a higher prevalence of bacterial GI infections in patients with NAFLD than those without (1.6% vs 0.9%, p< 0.001). The incidence of Clostridium difficile (1.3% vs. 0.8%, p< 0.001), Escherichia coli(0.3% vs. 0.01%, p< 0.001), as well as Salmonella (0.07% vs. 0.03%, p< 0.001) was higher in the NAFLD group compared to the non-NAFLD group . On univariate analysis, the presence of fatty liver was associated with a statistically significant higher odds of developing GI infections (aOR-1.75, 95% CI- 1.68-1.83, p< 0.001). After adjusting for confounding factors, the results remained statistically significant (aOR-1.38, 95% CI, p< 0.001)(Figure 1).
Discussion: Our study demonstrates an increase in risk of gastrointestinal infections in patients with NAFLD. Specifically, there was an increased risk of Clostridium difficile, Escherichia coli, and Salmonella. Prior studies have associated this risk to immune deficiencies and gut microbiota changes seen in NAFLD. Based on prior studies and our current results, we hypothesize that the immune and microbiota changes seen within NAFLD potentially contribute to the increased risk of gastrointestinal infections. Further prospective studies are needed to further clarify this association.

Disclosures:
Jay Patel, MD1, Aalam Sohal, MD2, Kanwal Bains, MBBS, CNSC3, Hunza Chaudhry, MD4, Isha Kohli, MBBS, CPH, MPH5, Kirti Arora, MBBS6, Shivam Kalra, MBBS7, Dino Dukovic, BS8, Marina Roytman, MD9. P0918 - Association of Non-Alcoholic Fatty Liver Disease With Gastrointestinal Infections: Insights From National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Orange Park Medical Center, Jacksonville, FL; 2Liver Institute Northwest, Seattle, WA; 3University of Arizona, Tucson, AZ; 4University of California San Francisco, Fresno, CA; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 7Trident Medical Center, Charleston, SC; 8Ross University School of Medicine, Maramar, FL; 9UCSF Fresno, Fresno, CA
Introduction: Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the world. NAFLD is associated with changes in the gut microbiota and has an interplay with the body’s immune response. These changes may contribute to increased risk of infections. The current study was aimed at assessing the relationship between the presence of NAFLD and the risk of bacterial gastrointestinal(GI) infections.
Methods: We queried the National Inpatient Sample (NIS) database in 2020 and stratified the patients based on presence of NAFLD. Information was collected regarding patient demographics, hospital characteristics, Charlson comorbidity Index, coexisting comorbidities(GERD,HLD, smoking, diabetes, hypertension, obesity, OSA, IBD), as well as bacterial gastrointestinal infections. Multivariate analysis was used to identify association between NAFLD and bacterial GI infections, after adjusting for confounding factors.
Results: A total of 26 million patients were admitted in 2020. Of these, 755,910 (2.85%) patients had the presence of NAFLD. The majority of the patients in the NAFLD group were over 65 years of age (46.1%), female (54.2%), had medicare (51.4%), and were in the lowest income quartile(30.9%)(Table 1). There was a higher prevalence of bacterial GI infections in patients with NAFLD than those without (1.6% vs 0.9%, p< 0.001). The incidence of Clostridium difficile (1.3% vs. 0.8%, p< 0.001), Escherichia coli(0.3% vs. 0.01%, p< 0.001), as well as Salmonella (0.07% vs. 0.03%, p< 0.001) was higher in the NAFLD group compared to the non-NAFLD group . On univariate analysis, the presence of fatty liver was associated with a statistically significant higher odds of developing GI infections (aOR-1.75, 95% CI- 1.68-1.83, p< 0.001). After adjusting for confounding factors, the results remained statistically significant (aOR-1.38, 95% CI, p< 0.001)(Figure 1).
Discussion: Our study demonstrates an increase in risk of gastrointestinal infections in patients with NAFLD. Specifically, there was an increased risk of Clostridium difficile, Escherichia coli, and Salmonella. Prior studies have associated this risk to immune deficiencies and gut microbiota changes seen in NAFLD. Based on prior studies and our current results, we hypothesize that the immune and microbiota changes seen within NAFLD potentially contribute to the increased risk of gastrointestinal infections. Further prospective studies are needed to further clarify this association.

Figure: Forest Plot depicting the associations between bacterial GI infections and study variables.
Table: Patient demographics, comorbidities, and presence of gastrointestinal infections, stratified by the presence of absence of underlying non-alcoholic fatty liver disease.
Disclosures:
Jay Patel indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Kanwal Bains indicated no relevant financial relationships.
Hunza Chaudhry indicated no relevant financial relationships.
Isha Kohli indicated no relevant financial relationships.
Kirti Arora indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Dino Dukovic indicated no relevant financial relationships.
Marina Roytman: Gilead – Advisor or Review Panel Member. Intercept – Advisor or Review Panel Member. VBI – Advisor or Review Panel Member.
Jay Patel, MD1, Aalam Sohal, MD2, Kanwal Bains, MBBS, CNSC3, Hunza Chaudhry, MD4, Isha Kohli, MBBS, CPH, MPH5, Kirti Arora, MBBS6, Shivam Kalra, MBBS7, Dino Dukovic, BS8, Marina Roytman, MD9. P0918 - Association of Non-Alcoholic Fatty Liver Disease With Gastrointestinal Infections: Insights From National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
