Sunday Poster Session
Category: Liver
P0928 - Efficacy of Zinc Supplementation in Hepatic Encephalopathy and Chronic Liver Disease: A Systematic Review and Meta-Analysis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- SA
Suchapa Arayakarnkul, MD
University of Minnesota
Minneapolis, Minnesota
Presenting Author(s)
Suchapa Arayakarnkul, MD1, Aunchalee Jaroenlapnopparat, MD2, Pongtawat Lertwilaiwittaya, MD3, Parth Patel, MD3
1University of Minnesota, Minneapolis, MN; 2Mount Auburn Hospital/Harvard Medical School, Cambridge, MA; 3University of Alabama at Birmingham, Birmingham, AL
Introduction: Zinc deficiency is associated with a worse prognosis in chronic liver disease (CLD), especially in setting of hepatic encephalopathy (HE). Zinc has the potential to ameliorate severity though ammonia conversion. This study aims to assess the benefits of oral zinc supplementation in the treatment of HE and the progression of CLD.
Methods: Pubmed Central, OVID Medline and EMBASE were searched from inception until May 2023 to identify studies that reported zinc supplementation, CLD and HE. Inclusion criteria were studies including CLD and/or HE patients who were given oral zinc, with or without comparison to a control group. Primary outcomes were the number connection test performance (NCT) and Child-Turcot-Pugh scores (CTP). Secondary outcomes included the serum ammonia levels, liver enzyme levels, and incidence of hepatocellular carcinoma (HCC).
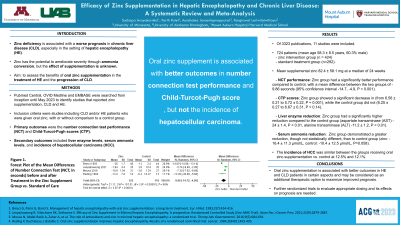
Results: 3323 publications were identified, of which 11 studies were included. A total of 724 patients (mean age 58.3 ± 8.5 years, 60.3% male), including those in the zinc intervention group (n = 424) and standard treatment group (n=292). Of the mean 82.4 ± 58.1 mg of supplemental zinc at a median of 24 weeks, the mean differences of NCT performance between the two groups were -9.86 seconds (95% confidence interval -14.7, -4.9, P < 0.001). The CTP scores showed a significant decrease in the zinc group (from 6.56 ± 0.21 to 5.72 ± 0.22, P = 0.001), while the control group did not (6.25 ± 0.27 to 6.67 ± 0.31, P = 0.14). Serum ammonia reduction was different, though not significantly, between the two groups (zinc: -16.4 ± 11.3 μmol/L, control: -10.4 ± 12.5 μmol/L, P=0.058). Differences in liver enzyme reduction was significantly higher in the zinc group compared to the control (aspartate transaminase (AST) -24 ± 1.4, P < 0.01, alanine transaminase (ALT) -11.2 ± 1.2, P < 0.01). The incidence of HCC was similar between the groups receiving oral zinc supplementation vs. control at 12.5% and 12.1%.
Discussion: This updated meta-analysis demonstrates oral zinc supplementation is associated with better outcomes in HE and CLD patients in certain aspects, and may be considered as an additional therapeutic option to maximize improved prognosis.

Disclosures:
Suchapa Arayakarnkul, MD1, Aunchalee Jaroenlapnopparat, MD2, Pongtawat Lertwilaiwittaya, MD3, Parth Patel, MD3. P0928 - Efficacy of Zinc Supplementation in Hepatic Encephalopathy and Chronic Liver Disease: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2Mount Auburn Hospital/Harvard Medical School, Cambridge, MA; 3University of Alabama at Birmingham, Birmingham, AL
Introduction: Zinc deficiency is associated with a worse prognosis in chronic liver disease (CLD), especially in setting of hepatic encephalopathy (HE). Zinc has the potential to ameliorate severity though ammonia conversion. This study aims to assess the benefits of oral zinc supplementation in the treatment of HE and the progression of CLD.
Methods: Pubmed Central, OVID Medline and EMBASE were searched from inception until May 2023 to identify studies that reported zinc supplementation, CLD and HE. Inclusion criteria were studies including CLD and/or HE patients who were given oral zinc, with or without comparison to a control group. Primary outcomes were the number connection test performance (NCT) and Child-Turcot-Pugh scores (CTP). Secondary outcomes included the serum ammonia levels, liver enzyme levels, and incidence of hepatocellular carcinoma (HCC).
Results: 3323 publications were identified, of which 11 studies were included. A total of 724 patients (mean age 58.3 ± 8.5 years, 60.3% male), including those in the zinc intervention group (n = 424) and standard treatment group (n=292). Of the mean 82.4 ± 58.1 mg of supplemental zinc at a median of 24 weeks, the mean differences of NCT performance between the two groups were -9.86 seconds (95% confidence interval -14.7, -4.9, P < 0.001). The CTP scores showed a significant decrease in the zinc group (from 6.56 ± 0.21 to 5.72 ± 0.22, P = 0.001), while the control group did not (6.25 ± 0.27 to 6.67 ± 0.31, P = 0.14). Serum ammonia reduction was different, though not significantly, between the two groups (zinc: -16.4 ± 11.3 μmol/L, control: -10.4 ± 12.5 μmol/L, P=0.058). Differences in liver enzyme reduction was significantly higher in the zinc group compared to the control (aspartate transaminase (AST) -24 ± 1.4, P < 0.01, alanine transaminase (ALT) -11.2 ± 1.2, P < 0.01). The incidence of HCC was similar between the groups receiving oral zinc supplementation vs. control at 12.5% and 12.1%.
Discussion: This updated meta-analysis demonstrates oral zinc supplementation is associated with better outcomes in HE and CLD patients in certain aspects, and may be considered as an additional therapeutic option to maximize improved prognosis.

Figure: Forest Plot of the Mean Differences of Number Connection Test (NCT, in seconds) before and after Treatment in the Zinc Supplement Group vs. Standard of Care
Disclosures:
Suchapa Arayakarnkul indicated no relevant financial relationships.
Aunchalee Jaroenlapnopparat indicated no relevant financial relationships.
Pongtawat Lertwilaiwittaya indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Suchapa Arayakarnkul, MD1, Aunchalee Jaroenlapnopparat, MD2, Pongtawat Lertwilaiwittaya, MD3, Parth Patel, MD3. P0928 - Efficacy of Zinc Supplementation in Hepatic Encephalopathy and Chronic Liver Disease: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
