Sunday Poster Session
Category: Liver
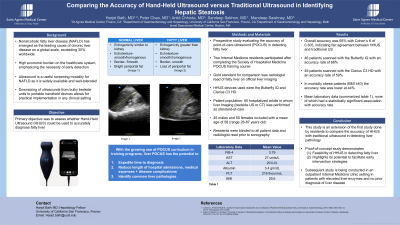
P0930 - Comparing the Accuracy of Hand-Held Ultrasound vs Traditional Ultrasound in Identifying Hepatic Steatosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Harjot Bath, MD
University of California San Francisco, Fresno
Fresno, CA
Presenting Author(s)
Harjot Bath, MD1, Peter Chao, MD2, Ankit Chhoda, MD3, Sandeep Sekhon, MD2, Mandeep Sawhney, MD, MS3
1University of California San Francisco, Fresno, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA; 3Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Nonalcoholic fatty liver disease (NAFLD) has emerged as the leading cause of chronic liver disease on a global scale. Its staggering prevalence exceeding 30% worldwide carries a substantial economic burden. Ultrasound (US) is a useful modality for identifying NAFLD as it is widely available and well-tolerated. Advancement in technology has enabled the downsizing of ultrasounds from bulky bedside units to portable handheld devices that allow for practical implementation.
Methods: We conducted a prospective study to evaluate the accuracy of point-of-care ultrasound (POCUS) in detecting fatty liver. Two Internal Medicine residents participated in completing the ultrasounds. They were trained through the Society of Hospitalist Medicine POCUS course. The primary objective was to assess whether HHUS could be used to accurately diagnose fatty liver. The gold standard for comparison was radiologist read of fatty liver on official liver imaging. HHUS devices used were the Butterfly iQ and Clarius C3 HD. Patient population included 95 hospitalized adults in whom liver imaging (bedside US or CT) was performed as standard-of-care. There were 45 males and 50 females included with a mean age of 58 (range 28-87 years old).Residents were blinded to all patient data and radiologist reads prior to sonography.
Results: Overall accuracy was 65% with Cohen’s K of 0.305, indicating fair agreement between HHUS and traditional US. This includes 7 patients for whom HHUS imaging data was missing due to device technical error, 3 patients for whom HHUS imaging quality was too poor for assessment, and 1 who lacked official liver imaging. There were 46 patients scanned with the Butterfly iQ with 3 lacking imaging due to technical errors, for an accuracy rate of 66%. There were 49 patients scanned with the Clarius C3 HD with 3 lacking imaging due to technical errors, for an accuracy rate of 59%. In morbidly obese patients (BMI ≥40) the accuracy rate was lower, 44%. Mean laboratory data included FIB-4 score 3.79, AST 27 units/L, ALT 29 IU/L, albumin 3.4 gm/dL, platelets 216 thou/mcL and BMI 29.6, none of which had a statistically significant association with accuracy rate.
Discussion: In conclusion, this study is an extension of the first study done by residents to compare the accuracy of HHUS with traditional ultrasound in detecting liver pathology. This proof-of-concept study demonstrates the feasibility of handheld US in detecting NAFLD and highlights its potential to facilitate early intervention strategies.
Disclosures:
Harjot Bath, MD1, Peter Chao, MD2, Ankit Chhoda, MD3, Sandeep Sekhon, MD2, Mandeep Sawhney, MD, MS3. P0930 - Comparing the Accuracy of Hand-Held Ultrasound vs Traditional Ultrasound in Identifying Hepatic Steatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California San Francisco, Fresno, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA; 3Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Nonalcoholic fatty liver disease (NAFLD) has emerged as the leading cause of chronic liver disease on a global scale. Its staggering prevalence exceeding 30% worldwide carries a substantial economic burden. Ultrasound (US) is a useful modality for identifying NAFLD as it is widely available and well-tolerated. Advancement in technology has enabled the downsizing of ultrasounds from bulky bedside units to portable handheld devices that allow for practical implementation.
Methods: We conducted a prospective study to evaluate the accuracy of point-of-care ultrasound (POCUS) in detecting fatty liver. Two Internal Medicine residents participated in completing the ultrasounds. They were trained through the Society of Hospitalist Medicine POCUS course. The primary objective was to assess whether HHUS could be used to accurately diagnose fatty liver. The gold standard for comparison was radiologist read of fatty liver on official liver imaging. HHUS devices used were the Butterfly iQ and Clarius C3 HD. Patient population included 95 hospitalized adults in whom liver imaging (bedside US or CT) was performed as standard-of-care. There were 45 males and 50 females included with a mean age of 58 (range 28-87 years old).Residents were blinded to all patient data and radiologist reads prior to sonography.
Results: Overall accuracy was 65% with Cohen’s K of 0.305, indicating fair agreement between HHUS and traditional US. This includes 7 patients for whom HHUS imaging data was missing due to device technical error, 3 patients for whom HHUS imaging quality was too poor for assessment, and 1 who lacked official liver imaging. There were 46 patients scanned with the Butterfly iQ with 3 lacking imaging due to technical errors, for an accuracy rate of 66%. There were 49 patients scanned with the Clarius C3 HD with 3 lacking imaging due to technical errors, for an accuracy rate of 59%. In morbidly obese patients (BMI ≥40) the accuracy rate was lower, 44%. Mean laboratory data included FIB-4 score 3.79, AST 27 units/L, ALT 29 IU/L, albumin 3.4 gm/dL, platelets 216 thou/mcL and BMI 29.6, none of which had a statistically significant association with accuracy rate.
Discussion: In conclusion, this study is an extension of the first study done by residents to compare the accuracy of HHUS with traditional ultrasound in detecting liver pathology. This proof-of-concept study demonstrates the feasibility of handheld US in detecting NAFLD and highlights its potential to facilitate early intervention strategies.
Disclosures:
Harjot Bath indicated no relevant financial relationships.
Peter Chao indicated no relevant financial relationships.
Ankit Chhoda indicated no relevant financial relationships.
Sandeep Sekhon indicated no relevant financial relationships.
Mandeep Sawhney: Allurion – Stock Options. Immunovia Inc. – Consultant. Marlborough, MA – Consultant.
Harjot Bath, MD1, Peter Chao, MD2, Ankit Chhoda, MD3, Sandeep Sekhon, MD2, Mandeep Sawhney, MD, MS3. P0930 - Comparing the Accuracy of Hand-Held Ultrasound vs Traditional Ultrasound in Identifying Hepatic Steatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

