Sunday Poster Session
Category: Liver
P0931 - Navigating Alcohol After Liver Transplant: Understanding Providers' Attitudes and Practices in Screening and Management
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Nghiem B. Ha, MD, MAS
University of California, San Francisco
San Francisco, CA
Presenting Author(s)
Nghiem B. Ha, MD, MAS1, Maria J. Duarte, MD1, Lisa X.. Deng, MD1, Rena Mei, MD1, Yejoo Jeon, MD1, Connie W. Wang, MD1, Triveni DeFries, MD2, Bilal Hameed, MD1, Courtney B. Sherman, MD1
1University of California, San Francisco, San Francisco, CA; 2San Francisco General Hospital, San Francisco, CA
Introduction: Alcohol-associated liver disease (ALD) is the leading indication for liver transplant (LT) though return to alcohol use occurs up to 22% by year 1 and is associated with poor post-LT outcomes. While alcohol screening along with abstinence-promoting behavioral and pharmacotherapy is the foundation in managing alcohol use disorder (AUD), it is underutilized in hepatology. We aim to examine provider attitudes and practice patterns in screening/management of alcohol use in post-LT patients.
Methods: We surveyed providers including GI/hep/LT fellows, hep/LT faculty, and APP at a single transplant center. The 13-question Likert survey assessed providers’ view and practice patterns in AUD screening and management.
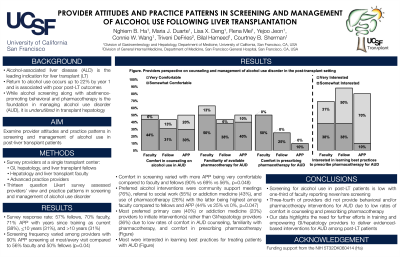
Results: Survey response rate: 57% fellows (16 of 28), 70% faculty (16 of 23), 71% APP (10 of 14) with years since training as 38% current, 31% <10, 31% >10 years. Although most (96%) felt that screening was important, frequency varied among providers with 90% APP screening at most/every visit compared to faculty and fellows (56% vs 50%, p=0.04); 31% of faculty reported never/rarely. Comfort in screening varied among providers with more APP being very comfortable compared to faculty and fellows (90% vs 69% vs 56%, p=0.048). 50% felt uncomfortable using DSM-V to diagnose AUD, particularly fellows (63%). Preferred interventions were community support meetings (76%), referral to social work (55%) or addiction medicine (43%), and use of pharmacotherapy (26%), with the latter being highest among faculty compared to fellows and APP (44% vs 25% vs 0%, p=0.047). Most preferred that primary care (40%) or addiction medicine (23%) initiate interventions rather than GI/hep providers (36%) due to low rates of comfort in AUD counseling (6% vs 13% vs 10%), familiarity with pharmacotherapy (13% vs 6% vs 10%) and discomfort in prescribing pharmacotherapy (38% vs 69% vs 90%, p=0.05) among faculty, fellows, and APP, respectively; though most (79%) were interested in learning best practices for treating ALD patients with AUD (Figure).
Discussion: Screening for alcohol use in post-LT patients is low with one-third of faculty reporting never/rare screening. Notably, three-fourth of providers did not provide behavioral and/or pharmacotherapy interventions for AUD due to low rates of comfort in counseling and prescribing pharmacotherapy. This data highlights the need for further efforts in training and empowering GI/hepatology providers to deliver evidenced-based interventions for AUD among post-LT patients.

Disclosures:
Nghiem B. Ha, MD, MAS1, Maria J. Duarte, MD1, Lisa X.. Deng, MD1, Rena Mei, MD1, Yejoo Jeon, MD1, Connie W. Wang, MD1, Triveni DeFries, MD2, Bilal Hameed, MD1, Courtney B. Sherman, MD1. P0931 - Navigating Alcohol After Liver Transplant: Understanding Providers' Attitudes and Practices in Screening and Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California, San Francisco, San Francisco, CA; 2San Francisco General Hospital, San Francisco, CA
Introduction: Alcohol-associated liver disease (ALD) is the leading indication for liver transplant (LT) though return to alcohol use occurs up to 22% by year 1 and is associated with poor post-LT outcomes. While alcohol screening along with abstinence-promoting behavioral and pharmacotherapy is the foundation in managing alcohol use disorder (AUD), it is underutilized in hepatology. We aim to examine provider attitudes and practice patterns in screening/management of alcohol use in post-LT patients.
Methods: We surveyed providers including GI/hep/LT fellows, hep/LT faculty, and APP at a single transplant center. The 13-question Likert survey assessed providers’ view and practice patterns in AUD screening and management.
Results: Survey response rate: 57% fellows (16 of 28), 70% faculty (16 of 23), 71% APP (10 of 14) with years since training as 38% current, 31% <10, 31% >10 years. Although most (96%) felt that screening was important, frequency varied among providers with 90% APP screening at most/every visit compared to faculty and fellows (56% vs 50%, p=0.04); 31% of faculty reported never/rarely. Comfort in screening varied among providers with more APP being very comfortable compared to faculty and fellows (90% vs 69% vs 56%, p=0.048). 50% felt uncomfortable using DSM-V to diagnose AUD, particularly fellows (63%). Preferred interventions were community support meetings (76%), referral to social work (55%) or addiction medicine (43%), and use of pharmacotherapy (26%), with the latter being highest among faculty compared to fellows and APP (44% vs 25% vs 0%, p=0.047). Most preferred that primary care (40%) or addiction medicine (23%) initiate interventions rather than GI/hep providers (36%) due to low rates of comfort in AUD counseling (6% vs 13% vs 10%), familiarity with pharmacotherapy (13% vs 6% vs 10%) and discomfort in prescribing pharmacotherapy (38% vs 69% vs 90%, p=0.05) among faculty, fellows, and APP, respectively; though most (79%) were interested in learning best practices for treating ALD patients with AUD (Figure).
Discussion: Screening for alcohol use in post-LT patients is low with one-third of faculty reporting never/rare screening. Notably, three-fourth of providers did not provide behavioral and/or pharmacotherapy interventions for AUD due to low rates of comfort in counseling and prescribing pharmacotherapy. This data highlights the need for further efforts in training and empowering GI/hepatology providers to deliver evidenced-based interventions for AUD among post-LT patients.

Figure: Providers' perspective on counseling and management of alcohol use disorder in the post-transplant setting
Disclosures:
Nghiem Ha indicated no relevant financial relationships.
Maria Duarte indicated no relevant financial relationships.
Lisa Deng indicated no relevant financial relationships.
Rena Mei indicated no relevant financial relationships.
Yejoo Jeon indicated no relevant financial relationships.
Connie Wang indicated no relevant financial relationships.
Triveni DeFries indicated no relevant financial relationships.
Bilal Hameed indicated no relevant financial relationships.
Courtney Sherman indicated no relevant financial relationships.
Nghiem B. Ha, MD, MAS1, Maria J. Duarte, MD1, Lisa X.. Deng, MD1, Rena Mei, MD1, Yejoo Jeon, MD1, Connie W. Wang, MD1, Triveni DeFries, MD2, Bilal Hameed, MD1, Courtney B. Sherman, MD1. P0931 - Navigating Alcohol After Liver Transplant: Understanding Providers' Attitudes and Practices in Screening and Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
