Sunday Poster Session
Category: Liver
P0936 - High-Risk Alcohol Use Is Associated With Significantly Greater Risk of Incident Hepatocellular Carcinoma in a National Cohort of U.S. Veterans With Metabolic Dysfunction Associated Fatty Liver Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Robert J. Wong, MD, MS, FACG
Stanford/VA Palo Alto
Palo Alto, CA
Presenting Author(s)
Award: Presidential Poster Award
Robert J.. Wong, MD, MS, FACG1, Zeyuan Yang, MSc2, Ramsey Cheung, MD1, Ashwani K. Singal, MD, MS, FACG3, Albert Do, MD, MPH4, Aijaz Ahmed, MD5, Aaron Yeoh, MD5
1Stanford/VA Palo Alto, Palo Alto, CA; 2VA Palo Alto, Palo Alto, CA; 3University of South Dakota, Sioux Falls, SD; 4Yale School of Medicine, New Haven, CT; 5Stanford, Palo Alto, CA
Introduction: Metabolic dysfunction associated fatty liver disease (MAFLD) is highly prevalent among U.S. Veterans, a population enriched in metabolic co-morbidities. Conflicting data exists on the impact of different levels of alcohol use on risk of disease progression in fatty liver; few data have specifically evaluated this in MAFLD. We evaluated the association between levels of alcohol use and risk of hepatocellular carcinoma (HCC) among a national cohort of Veterans with MAFLD.
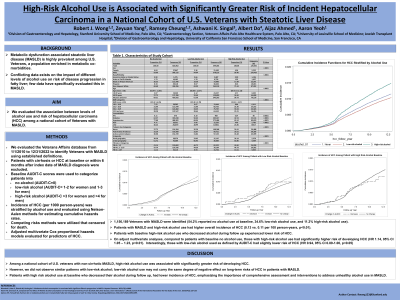
Methods: We evaluated the Veterans Affairs database from 1/1/2010 to 12/31/2022 to identify Veterans with MAFLD using established definitions. Patients with cirrhosis or HCC at baseline or within 6 months after index date of MAFLD diagnosis were excluded. Baseline AUDIT-C scores were used to categorize patients into no alcohol (AUDIT-C=0), low-risk alcohol (AUDIT-C= 1-2 for women and 1-3 for men), and high-risk alcohol (AUDIT-C >3 for women and >4 for men). Incidence of HCC (per 1000 person-years) was stratified by alcohol use and evaluated using Nelson-Aalen methods for estimating cumulative hazards rates. We applied competing risks methods that censored for death. Adjusted multivariate Cox proportional hazards models evaluated for predictors of HCC.
Results: Among 1,156,189 Veterans with MAFLD, 54.2% reported no alcohol use, 34.6% low-risk alcohol, and 11.2% high-risk alcohol. Compared to patients with no alcohol, high-risk alcohol users were younger (59.9y vs. 64.0y, p< 0.01), had lower proportion with diabetes (42.5% vs. 62.4%, p< 0.01), but had higher FIB-4 scores at baseline (proportion with FIB-4 >2.67: 15.0% vs. 11.1%, p< 0.01). Compared to MAFLD patients with no alcohol use, HCC incidence was significantly higher in patients with high-risk alcohol (1.29 vs. 1.09 per 1000 person-years, p< 0.01), but lower in patients with low-risk alcohol (0.89 vs. 1.09 per 1000 person-years, p< 0.01). On adjusted multivariate regression, compared to MAFLD patients with no alcohol, those with high-risk alcohol use had greater risk of HCC (HR 1.15, 95% CI 1.06-1.24); there was a trend towards slightly lower HCC risk in patients with low-risk alcohol use (HR 0.95, 95% CI 0.89-1.00).
Discussion: Among a national cohort of U.S. veterans with non-cirrhotic MAFLD, high-risk alcohol use was associated with significantly greater risk of developing HCC. However, we did not observe similar patterns with low-risk alcohol; low-risk alcohol use may not carry the same degree of negative effect on long-term risks of HCC in patients with MAFLD.

Disclosures:
Robert J.. Wong, MD, MS, FACG1, Zeyuan Yang, MSc2, Ramsey Cheung, MD1, Ashwani K. Singal, MD, MS, FACG3, Albert Do, MD, MPH4, Aijaz Ahmed, MD5, Aaron Yeoh, MD5. P0936 - High-Risk Alcohol Use Is Associated With Significantly Greater Risk of Incident Hepatocellular Carcinoma in a National Cohort of U.S. Veterans With Metabolic Dysfunction Associated Fatty Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Robert J.. Wong, MD, MS, FACG1, Zeyuan Yang, MSc2, Ramsey Cheung, MD1, Ashwani K. Singal, MD, MS, FACG3, Albert Do, MD, MPH4, Aijaz Ahmed, MD5, Aaron Yeoh, MD5
1Stanford/VA Palo Alto, Palo Alto, CA; 2VA Palo Alto, Palo Alto, CA; 3University of South Dakota, Sioux Falls, SD; 4Yale School of Medicine, New Haven, CT; 5Stanford, Palo Alto, CA
Introduction: Metabolic dysfunction associated fatty liver disease (MAFLD) is highly prevalent among U.S. Veterans, a population enriched in metabolic co-morbidities. Conflicting data exists on the impact of different levels of alcohol use on risk of disease progression in fatty liver; few data have specifically evaluated this in MAFLD. We evaluated the association between levels of alcohol use and risk of hepatocellular carcinoma (HCC) among a national cohort of Veterans with MAFLD.
Methods: We evaluated the Veterans Affairs database from 1/1/2010 to 12/31/2022 to identify Veterans with MAFLD using established definitions. Patients with cirrhosis or HCC at baseline or within 6 months after index date of MAFLD diagnosis were excluded. Baseline AUDIT-C scores were used to categorize patients into no alcohol (AUDIT-C=0), low-risk alcohol (AUDIT-C= 1-2 for women and 1-3 for men), and high-risk alcohol (AUDIT-C >3 for women and >4 for men). Incidence of HCC (per 1000 person-years) was stratified by alcohol use and evaluated using Nelson-Aalen methods for estimating cumulative hazards rates. We applied competing risks methods that censored for death. Adjusted multivariate Cox proportional hazards models evaluated for predictors of HCC.
Results: Among 1,156,189 Veterans with MAFLD, 54.2% reported no alcohol use, 34.6% low-risk alcohol, and 11.2% high-risk alcohol. Compared to patients with no alcohol, high-risk alcohol users were younger (59.9y vs. 64.0y, p< 0.01), had lower proportion with diabetes (42.5% vs. 62.4%, p< 0.01), but had higher FIB-4 scores at baseline (proportion with FIB-4 >2.67: 15.0% vs. 11.1%, p< 0.01). Compared to MAFLD patients with no alcohol use, HCC incidence was significantly higher in patients with high-risk alcohol (1.29 vs. 1.09 per 1000 person-years, p< 0.01), but lower in patients with low-risk alcohol (0.89 vs. 1.09 per 1000 person-years, p< 0.01). On adjusted multivariate regression, compared to MAFLD patients with no alcohol, those with high-risk alcohol use had greater risk of HCC (HR 1.15, 95% CI 1.06-1.24); there was a trend towards slightly lower HCC risk in patients with low-risk alcohol use (HR 0.95, 95% CI 0.89-1.00).
Discussion: Among a national cohort of U.S. veterans with non-cirrhotic MAFLD, high-risk alcohol use was associated with significantly greater risk of developing HCC. However, we did not observe similar patterns with low-risk alcohol; low-risk alcohol use may not carry the same degree of negative effect on long-term risks of HCC in patients with MAFLD.

Figure: Figure. Cumulative Incidence of Hepatocellular Carcinoma in Patients with Non-Cirrhotic MAFLD Stratified by Alcohol Use
Disclosures:
Robert Wong: Exact Sciences – Grant/Research Support. Gilead Sciences – Consultant, Grant/Research Support. Thera Technologies – Grant/Research Support.
Zeyuan Yang indicated no relevant financial relationships.
Ramsey Cheung indicated no relevant financial relationships.
Ashwani K. Singal indicated no relevant financial relationships.
Albert Do indicated no relevant financial relationships.
Aijaz Ahmed indicated no relevant financial relationships.
Aaron Yeoh indicated no relevant financial relationships.
Robert J.. Wong, MD, MS, FACG1, Zeyuan Yang, MSc2, Ramsey Cheung, MD1, Ashwani K. Singal, MD, MS, FACG3, Albert Do, MD, MPH4, Aijaz Ahmed, MD5, Aaron Yeoh, MD5. P0936 - High-Risk Alcohol Use Is Associated With Significantly Greater Risk of Incident Hepatocellular Carcinoma in a National Cohort of U.S. Veterans With Metabolic Dysfunction Associated Fatty Liver Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

