Sunday Poster Session
Category: Liver
P0981 - Cardiovascular Death and Liver Disease: Mortality Trends and Disparities
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- RT
Richard Trieu, MD
University of Arizona–Banner University Medical Center
Tucson, AZ
Presenting Author(s)
Richard Trieu, MD1, Elise Le Cam, MD1, Macklin Loveland, MD2, Ala Kasrawi, MD3, Kristina Terrani, MS4, Mohammed Salih, MD5, Ramzi Ibrahim, MD4
1University of Arizona–Banner University Medical Center, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ; 3Jordanian Royal Medical Services, Amman, 'Amman, Jordan; 4University of Arizona, Tucson, AZ; 5Baylor University Medical Center, The Heart Hospital, Plano, TX
Introduction: Liver disease often coexists with cardiovascular disease (CVD), resulting in increased morbidity and mortality. Understanding contemporary disparities through population-based research is crucial for promoting healthcare equity. In this study, we aimed to investigate trends in CVD-related mortality among individuals with liver disease.
Methods: Data were obtained from the Centers for Disease Control and Prevention (CDC) Wide Ranging Online Data for Epidemiologic Research database, which captures United States mortality data using death certificate diagnoses and demographic information. We queried CVD-related mortality as the underlying cause of death with liver disease as a contributing cause from 1999 to 2020. Age-adjusted mortality rates (AAMR), average annual percentage change (AAPC), and 95% confidence intervals (CI) were quantified. Subgroup analyses were conducted based on gender, race, and geographic information. To evaluate mortality trends, log-linear regression models were utilized, and statistical significance was determined using a two-tailed t-test with a significance level set at p< 0.05.
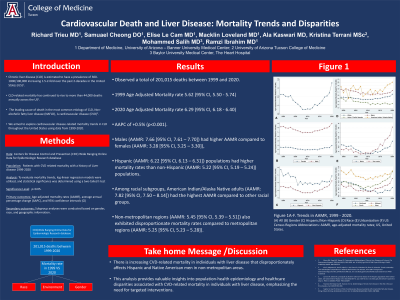
Results: We observed a total of 201,015 deaths between 1999 and 2020. The AAMR increased from 5.62 (95% CI, 5.50 - 5.74) in 1999 to 6.29 (95% CI, 6.18 - 6.40) in 2020, with an AAPC of +0.5% (p< 0.001). Males (AAMR: 7.66 [95% CI, 7.61 – 7.70]) had higher AAMR compared to females (AAMR: 3.28 [95% CI, 3.25 – 3.30]), and Hispanic (AAMR: 6.22 [95% CI, 6.13 – 6.31]) populations had higher mortality rates than non-Hispanic (AAMR: 5.22 [95% CI, 5.19 – 5.24]) populations. Among racial subgroups, American Indian/Alaska Native adults (AAMR: 7.82 [95% CI, 7.50 – 8.14]) had the highest AAMR compared to other racial groups. Non-metropolitan regions (AAMR: 5.45 [95% CI, 5.39 – 5.51]) also exhibited disproportionate mortality rates compared to metropolitan regions (AAMR: 5.25 [95% CI, 5.23 – 5.28]).
Discussion: The findings highlight the increasing CVD-related mortality in individuals with liver disease and the disparities among different gender, racial, and geographic subgroups. This analysis provides valuable insights into population-health epidemiology and healthcare disparities associated with CVD-related mortality in individuals with liver disease, emphasizing the need for targeted interventions.

Disclosures:
Richard Trieu, MD1, Elise Le Cam, MD1, Macklin Loveland, MD2, Ala Kasrawi, MD3, Kristina Terrani, MS4, Mohammed Salih, MD5, Ramzi Ibrahim, MD4. P0981 - Cardiovascular Death and Liver Disease: Mortality Trends and Disparities, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona–Banner University Medical Center, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ; 3Jordanian Royal Medical Services, Amman, 'Amman, Jordan; 4University of Arizona, Tucson, AZ; 5Baylor University Medical Center, The Heart Hospital, Plano, TX
Introduction: Liver disease often coexists with cardiovascular disease (CVD), resulting in increased morbidity and mortality. Understanding contemporary disparities through population-based research is crucial for promoting healthcare equity. In this study, we aimed to investigate trends in CVD-related mortality among individuals with liver disease.
Methods: Data were obtained from the Centers for Disease Control and Prevention (CDC) Wide Ranging Online Data for Epidemiologic Research database, which captures United States mortality data using death certificate diagnoses and demographic information. We queried CVD-related mortality as the underlying cause of death with liver disease as a contributing cause from 1999 to 2020. Age-adjusted mortality rates (AAMR), average annual percentage change (AAPC), and 95% confidence intervals (CI) were quantified. Subgroup analyses were conducted based on gender, race, and geographic information. To evaluate mortality trends, log-linear regression models were utilized, and statistical significance was determined using a two-tailed t-test with a significance level set at p< 0.05.
Results: We observed a total of 201,015 deaths between 1999 and 2020. The AAMR increased from 5.62 (95% CI, 5.50 - 5.74) in 1999 to 6.29 (95% CI, 6.18 - 6.40) in 2020, with an AAPC of +0.5% (p< 0.001). Males (AAMR: 7.66 [95% CI, 7.61 – 7.70]) had higher AAMR compared to females (AAMR: 3.28 [95% CI, 3.25 – 3.30]), and Hispanic (AAMR: 6.22 [95% CI, 6.13 – 6.31]) populations had higher mortality rates than non-Hispanic (AAMR: 5.22 [95% CI, 5.19 – 5.24]) populations. Among racial subgroups, American Indian/Alaska Native adults (AAMR: 7.82 [95% CI, 7.50 – 8.14]) had the highest AAMR compared to other racial groups. Non-metropolitan regions (AAMR: 5.45 [95% CI, 5.39 – 5.51]) also exhibited disproportionate mortality rates compared to metropolitan regions (AAMR: 5.25 [95% CI, 5.23 – 5.28]).
Discussion: The findings highlight the increasing CVD-related mortality in individuals with liver disease and the disparities among different gender, racial, and geographic subgroups. This analysis provides valuable insights into population-health epidemiology and healthcare disparities associated with CVD-related mortality in individuals with liver disease, emphasizing the need for targeted interventions.

Figure: Figure 1A-F. Trends in AAMR, 1999 - 2020. (A) All (B) Gender (C) Hispanic/Non-Hispanic (D) Race (E) Urbanization (F) US Census Regions
Abbreviations: AAMR, age-adjusted mortality rates; US, United States.
Abbreviations: AAMR, age-adjusted mortality rates; US, United States.
Disclosures:
Richard Trieu indicated no relevant financial relationships.
Elise Le Cam indicated no relevant financial relationships.
Macklin Loveland indicated no relevant financial relationships.
Ala Kasrawi indicated no relevant financial relationships.
Kristina Terrani indicated no relevant financial relationships.
Mohammed Salih indicated no relevant financial relationships.
Ramzi Ibrahim indicated no relevant financial relationships.
Richard Trieu, MD1, Elise Le Cam, MD1, Macklin Loveland, MD2, Ala Kasrawi, MD3, Kristina Terrani, MS4, Mohammed Salih, MD5, Ramzi Ibrahim, MD4. P0981 - Cardiovascular Death and Liver Disease: Mortality Trends and Disparities, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
