Sunday Poster Session
Category: Liver
P0985 - Revolutionary Defense: Evusheld Triumphs in Combating Post Covid-ILD Among Liver and Kidney Transplant Recipients
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AC
Ammad J. Chaudhary, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Ammad Chaudhary, MD1, Hamna Fahad, MD1, Momin Samad, MD2, Sheema Rehman, DO1, Ashley Francis, BS3, Hope Baldwin, 3, Fariba Rana, 3, Umer Farooq, MD4, Yervant Ichkhanian, MD1, Syed-Mohammed Jafri, MD5
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Rochester Hills, MI; 3Wayne State University, Detroit, MI; 4University of Rochester, Rochester, NY; 5Henry Ford Health System, Detroit, MI
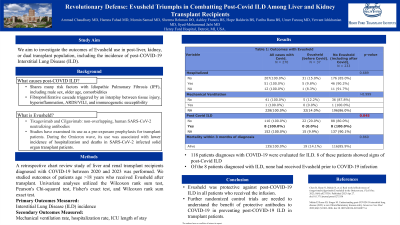
Introduction: The COVID-19 pandemic has not only caused immediate morbidity and mortality but has also been linked to residual chronic cardio-pulmonary sequelae. Literature shows that patients with severe COVID-19 pneumonia have a higher risk of developing interstitial lung disease (ILD) and chronic pulmonary vascular disease, with Idiopathic Pulmonary Fibrosis being most closely associated with the pandemic. This devastating condition leads to a severe decline in lung function, respiratory failure, and eventually death unless rescued by lung transplantation. To optimize post-discharge care of COVID-19 patients, this study aimed to investigate the outcomes of Evusheld use in post-liver, kidney, or dual transplant population, including the incidence of post-COVID-19 ILD.
Methods:
This retrospective chart review study was conducted at a tertiary care center from 2022 to 2023. Adult patients (age > 18 years) who received Evusheld after liver, kidney, or simultaneous liver-kidney transplant were included. Demographics, disease characteristics, and outcomes were recorded in de-identified datasheets. The primary outcome measured was the incidence of positive COVID-19 PCR tests. Secondary outcomes included the progression to interstitial lung disease (ILD), mechanical ventilation rate, and hospitalization rate. Univariate analyses utilized the Wilcoxon rank sum test, Pearson's Chi-squared test, Fisher's exact test, and Wilcoxon rank sum exact test.
Results:
Among 1,151 solid organ transplant recipients, 273 (23.7%) were diagnosed with COVID-19 between the start of the pandemic and February 2023. Among these, 1,019 (88.5%) were offered Evusheld, and 379 (37.2%) received at least one dose of Evusheld during the period from 2022 to 2023. Out of these, 118 patients were evaluated for ILD. In total, 8 (6.7%) patients showed sequelae of post-COVID-19 ILD. None of these patients had received Evusheld prior to the COVID-19 infection (p < 0.05). Additionally, there was no significant difference in the rate of hospitalization, the need for mechanical ventilation, and the number of days spent in the ICU.
Discussion: Our results suggest that Evusheld was protective against post-COVID-19 ILD in all patients who received the infusion. The study is crucial, as it offers insight into the currently evolving care of COVID-19 survivors. Further randomized control trials are needed to understand the benefit of protective antibodies to COVID-19 in preventing post-COVID-19 ILD in transplant patients.
Disclosures:
Ammad Chaudhary, MD1, Hamna Fahad, MD1, Momin Samad, MD2, Sheema Rehman, DO1, Ashley Francis, BS3, Hope Baldwin, 3, Fariba Rana, 3, Umer Farooq, MD4, Yervant Ichkhanian, MD1, Syed-Mohammed Jafri, MD5. P0985 - Revolutionary Defense: Evusheld Triumphs in Combating Post Covid-ILD Among Liver and Kidney Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Rochester Hills, MI; 3Wayne State University, Detroit, MI; 4University of Rochester, Rochester, NY; 5Henry Ford Health System, Detroit, MI
Introduction: The COVID-19 pandemic has not only caused immediate morbidity and mortality but has also been linked to residual chronic cardio-pulmonary sequelae. Literature shows that patients with severe COVID-19 pneumonia have a higher risk of developing interstitial lung disease (ILD) and chronic pulmonary vascular disease, with Idiopathic Pulmonary Fibrosis being most closely associated with the pandemic. This devastating condition leads to a severe decline in lung function, respiratory failure, and eventually death unless rescued by lung transplantation. To optimize post-discharge care of COVID-19 patients, this study aimed to investigate the outcomes of Evusheld use in post-liver, kidney, or dual transplant population, including the incidence of post-COVID-19 ILD.
Methods:
This retrospective chart review study was conducted at a tertiary care center from 2022 to 2023. Adult patients (age > 18 years) who received Evusheld after liver, kidney, or simultaneous liver-kidney transplant were included. Demographics, disease characteristics, and outcomes were recorded in de-identified datasheets. The primary outcome measured was the incidence of positive COVID-19 PCR tests. Secondary outcomes included the progression to interstitial lung disease (ILD), mechanical ventilation rate, and hospitalization rate. Univariate analyses utilized the Wilcoxon rank sum test, Pearson's Chi-squared test, Fisher's exact test, and Wilcoxon rank sum exact test.
Results:
Among 1,151 solid organ transplant recipients, 273 (23.7%) were diagnosed with COVID-19 between the start of the pandemic and February 2023. Among these, 1,019 (88.5%) were offered Evusheld, and 379 (37.2%) received at least one dose of Evusheld during the period from 2022 to 2023. Out of these, 118 patients were evaluated for ILD. In total, 8 (6.7%) patients showed sequelae of post-COVID-19 ILD. None of these patients had received Evusheld prior to the COVID-19 infection (p < 0.05). Additionally, there was no significant difference in the rate of hospitalization, the need for mechanical ventilation, and the number of days spent in the ICU.
Discussion: Our results suggest that Evusheld was protective against post-COVID-19 ILD in all patients who received the infusion. The study is crucial, as it offers insight into the currently evolving care of COVID-19 survivors. Further randomized control trials are needed to understand the benefit of protective antibodies to COVID-19 in preventing post-COVID-19 ILD in transplant patients.
Disclosures:
Ammad Chaudhary indicated no relevant financial relationships.
Hamna Fahad indicated no relevant financial relationships.
Momin Samad indicated no relevant financial relationships.
Sheema Rehman indicated no relevant financial relationships.
Ashley Francis indicated no relevant financial relationships.
Hope Baldwin indicated no relevant financial relationships.
Fariba Rana indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Yervant Ichkhanian indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie – Advisor or Review Panel Member, Speakers Bureau.
Ammad Chaudhary, MD1, Hamna Fahad, MD1, Momin Samad, MD2, Sheema Rehman, DO1, Ashley Francis, BS3, Hope Baldwin, 3, Fariba Rana, 3, Umer Farooq, MD4, Yervant Ichkhanian, MD1, Syed-Mohammed Jafri, MD5. P0985 - Revolutionary Defense: Evusheld Triumphs in Combating Post Covid-ILD Among Liver and Kidney Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
