Sunday Poster Session
Category: Liver
P1020 - New Onset Autoimmune Hepatitis in a Patient Presenting With Abdominal Pain and Abnormal Liver Chemistries
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aria Jalalian, MD
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Aria Jalalian, MD1, Rachael Schneider, DO1, Stefanie Gallagher, DO1, Romy Chamoun, MD1, Roy Taoutel, MD1, Babak Etemad, MD2
1Lankenau Medical Center, Wynnewood, PA; 2Lankenau Medical Center, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic liver disease characterized by immune-mediated hepatocellular injury, which can lead to progressive liver damage and cirrhosis. AIH is characterized by elevated immunoglobulin G (IgG) levels, detectable autoantibodies, and interface hepatitis. We present the case of a 67-year-old female who presented with abdominal pain and abnormal liver chemistries, found to have AIH.
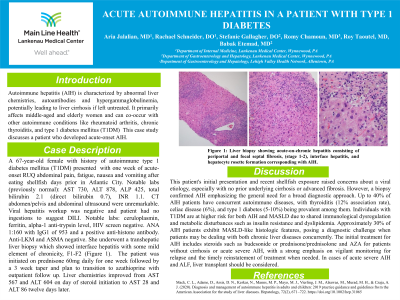
Case Description/Methods: A 67-year-old female with a past history of asthma and type 1 diabetes presented to the hospital with one week of progressive right upper quadrant abdominal pain, nausea, and vomiting. Notably, she had consumed shellfish and oysters at her birthday party a few weeks prior. She denied changing her bowel habits, fever, chills, or weight loss. Labs notable for AST 730, ALT 878, ALP 425, and total bilirubin 2.1 with a direct component 0.7, INR 1.1. CT abdomen/pelvis and abdominal ultrasound were without evidence of ductal dilation or cholestasis. Initially, her symptoms and labs were concerning for hepatitis A infection. However, her workup including an acute hepatitis panel was negative, and further workup revealed an unremarkable ceruloplasmin, ferritin, alpha-1 anti-trypsin level, and HIV screen. Continued testing then divulged an ANA 1:160 with positive IgG1 subclass and a positive anti-histone antibody. She underwent a liver biopsy which portrayed acute-on-chronic hepatitis with portal fibrosis (Figure 1). She was initiated on prednisone daily with improvement in her symptoms and of her abnormal liver chemistries. This patient had recovered one year after diagnosis after remaining on low-dose prednisone and azathioprine with consistently normal liver chemistries without evidence of progressive fibrosis on imaging.
Discussion: AIH is a progressive disease that warrants prompt diagnosis due to its pathologic sensitivity to immunosuppressive therapy. This case highlights the notion of maintaining a broad differential diagnosis when evaluating for a potential liver illness. When detected, quick initiation of therapy and close monitoring are important for prevention of progression to end-stage liver disease. The pathogenesis of AIH is thought to be multifactorial with a combination of genetic susceptibility, an impaired immune system, and molecular mimicry. Our case demonstrates the importance of sending an appropriate serologic workup and a low threshold to include an antibody screen in initial testing with consideration of AIH as a potential etiology.

Disclosures:
Aria Jalalian, MD1, Rachael Schneider, DO1, Stefanie Gallagher, DO1, Romy Chamoun, MD1, Roy Taoutel, MD1, Babak Etemad, MD2. P1020 - New Onset Autoimmune Hepatitis in a Patient Presenting With Abdominal Pain and Abnormal Liver Chemistries, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lankenau Medical Center, Wynnewood, PA; 2Lankenau Medical Center, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic liver disease characterized by immune-mediated hepatocellular injury, which can lead to progressive liver damage and cirrhosis. AIH is characterized by elevated immunoglobulin G (IgG) levels, detectable autoantibodies, and interface hepatitis. We present the case of a 67-year-old female who presented with abdominal pain and abnormal liver chemistries, found to have AIH.
Case Description/Methods: A 67-year-old female with a past history of asthma and type 1 diabetes presented to the hospital with one week of progressive right upper quadrant abdominal pain, nausea, and vomiting. Notably, she had consumed shellfish and oysters at her birthday party a few weeks prior. She denied changing her bowel habits, fever, chills, or weight loss. Labs notable for AST 730, ALT 878, ALP 425, and total bilirubin 2.1 with a direct component 0.7, INR 1.1. CT abdomen/pelvis and abdominal ultrasound were without evidence of ductal dilation or cholestasis. Initially, her symptoms and labs were concerning for hepatitis A infection. However, her workup including an acute hepatitis panel was negative, and further workup revealed an unremarkable ceruloplasmin, ferritin, alpha-1 anti-trypsin level, and HIV screen. Continued testing then divulged an ANA 1:160 with positive IgG1 subclass and a positive anti-histone antibody. She underwent a liver biopsy which portrayed acute-on-chronic hepatitis with portal fibrosis (Figure 1). She was initiated on prednisone daily with improvement in her symptoms and of her abnormal liver chemistries. This patient had recovered one year after diagnosis after remaining on low-dose prednisone and azathioprine with consistently normal liver chemistries without evidence of progressive fibrosis on imaging.
Discussion: AIH is a progressive disease that warrants prompt diagnosis due to its pathologic sensitivity to immunosuppressive therapy. This case highlights the notion of maintaining a broad differential diagnosis when evaluating for a potential liver illness. When detected, quick initiation of therapy and close monitoring are important for prevention of progression to end-stage liver disease. The pathogenesis of AIH is thought to be multifactorial with a combination of genetic susceptibility, an impaired immune system, and molecular mimicry. Our case demonstrates the importance of sending an appropriate serologic workup and a low threshold to include an antibody screen in initial testing with consideration of AIH as a potential etiology.

Figure: Figure 1: Liver biopsy showing acute-on-chronic hepatitis consisting of portal fibrosis, interface hepatitis, and hepatocyte rosette formation corresponding with AIH.
Disclosures:
Aria Jalalian indicated no relevant financial relationships.
Rachael Schneider indicated no relevant financial relationships.
Stefanie Gallagher indicated no relevant financial relationships.
Romy Chamoun indicated no relevant financial relationships.
Roy Taoutel indicated no relevant financial relationships.
Babak Etemad indicated no relevant financial relationships.
Aria Jalalian, MD1, Rachael Schneider, DO1, Stefanie Gallagher, DO1, Romy Chamoun, MD1, Roy Taoutel, MD1, Babak Etemad, MD2. P1020 - New Onset Autoimmune Hepatitis in a Patient Presenting With Abdominal Pain and Abnormal Liver Chemistries, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
