Sunday Poster Session
Category: Liver
P1028 - A Unique Case of Biliary Necrosis and Arterial Complications Following Two Orthotopic Liver Transplants
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Kevin Cobty, BS
Wayne State University School of Medicine
Detroit, MI
Presenting Author(s)
Kevin Cobty, BS1, Syed-Mohammed Jafri, MD2
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a rare case of hepatic artery thrombosis leading to biliary necrosis complicating two different orthotopic liver transplants (OLT) in a single patient.
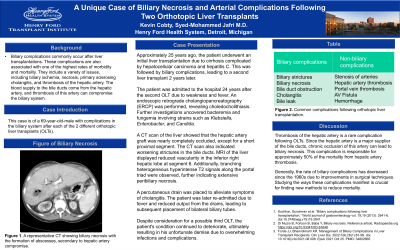
Case Description/Methods: A 69-year-old male with a history of two separate OLTs presents with decompensation. He underwent initial liver transplantation with Roux-en-Y hepaticojejunostomy 25 years ago due to hepatitis C, cirrhosis, and hepatocellular carcinoma. Two years later, after complications in the biliary system, a second liver transplant was performed. Approximately 24 years later, an endoscopic retrograde cholangiopancreatography was performed, and the patient was diagnosed with choledocholithiasis. He was admitted to the hospital 5 months ago due to weakness and fever from sepsis. Blood culture revealed bacteremia and fungemia, including Klebsiella, Enterobacter, and Candida, which progressed for months. A CT of the liver demonstrated that the hepatic artery graft was almost entirely occluded, except for the proximal short segment portion. The CT showed diffuse branching hypoattenuating structures that followed the bile ducts. When compared to other CT scans taken a few weeks prior, these structures continuously increased, reflecting worsening biliary necrosis. A percutaneous biliary drain was placed by Interventional Radiology to relieve symptoms from cholangitis. A few weeks later, an MRI of the liver demonstrated decreased vascularity in the inferior right hepatic lobe at segment 6. No evidence of steatosis was found. The MRI also showed branching heterogenous hyperintense T2 signals along the portal triad, showing further signs of extensive peribiliary necrosis. Three months ago, the patient underwent a procedure to add a second internal/external biliary drain. A month later, the patient was re-admitted to the hospital due to fever and decreased output from one of the drains. Subsequently, he underwent a bilateral biliary tube replacement. He was evaluated for a possible third OLT, but due to infections and debility, he was not listed. After overwhelming complications and infections, the patient passed away.
Discussion: Hepatic artery thrombosis is a rare complication of OLTs. If chronic occlusion occurs, a serious possible result that can occur is biliary necrosis. This is responsible for approximately 50% of the mortality from hepatic artery thrombosis. Studying how this complication manifests is crucial to finding treatments that will ultimately reduce mortality.
Disclosures:
Kevin Cobty, BS1, Syed-Mohammed Jafri, MD2. P1028 - A Unique Case of Biliary Necrosis and Arterial Complications Following Two Orthotopic Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a rare case of hepatic artery thrombosis leading to biliary necrosis complicating two different orthotopic liver transplants (OLT) in a single patient.
Case Description/Methods: A 69-year-old male with a history of two separate OLTs presents with decompensation. He underwent initial liver transplantation with Roux-en-Y hepaticojejunostomy 25 years ago due to hepatitis C, cirrhosis, and hepatocellular carcinoma. Two years later, after complications in the biliary system, a second liver transplant was performed. Approximately 24 years later, an endoscopic retrograde cholangiopancreatography was performed, and the patient was diagnosed with choledocholithiasis. He was admitted to the hospital 5 months ago due to weakness and fever from sepsis. Blood culture revealed bacteremia and fungemia, including Klebsiella, Enterobacter, and Candida, which progressed for months. A CT of the liver demonstrated that the hepatic artery graft was almost entirely occluded, except for the proximal short segment portion. The CT showed diffuse branching hypoattenuating structures that followed the bile ducts. When compared to other CT scans taken a few weeks prior, these structures continuously increased, reflecting worsening biliary necrosis. A percutaneous biliary drain was placed by Interventional Radiology to relieve symptoms from cholangitis. A few weeks later, an MRI of the liver demonstrated decreased vascularity in the inferior right hepatic lobe at segment 6. No evidence of steatosis was found. The MRI also showed branching heterogenous hyperintense T2 signals along the portal triad, showing further signs of extensive peribiliary necrosis. Three months ago, the patient underwent a procedure to add a second internal/external biliary drain. A month later, the patient was re-admitted to the hospital due to fever and decreased output from one of the drains. Subsequently, he underwent a bilateral biliary tube replacement. He was evaluated for a possible third OLT, but due to infections and debility, he was not listed. After overwhelming complications and infections, the patient passed away.
Discussion: Hepatic artery thrombosis is a rare complication of OLTs. If chronic occlusion occurs, a serious possible result that can occur is biliary necrosis. This is responsible for approximately 50% of the mortality from hepatic artery thrombosis. Studying how this complication manifests is crucial to finding treatments that will ultimately reduce mortality.
Disclosures:
Kevin Cobty indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie – Advisor or Review Panel Member, Speakers Bureau.
Kevin Cobty, BS1, Syed-Mohammed Jafri, MD2. P1028 - A Unique Case of Biliary Necrosis and Arterial Complications Following Two Orthotopic Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
